Editor's note: This is part three of a three-part series. Read part one here. Read part two here.
In parts one and two of this series, I described how the introduction of the medical management of tooth decay with silver diamine fluoride (SDF) impacted several major practice metrics. Examples include the increase in total patients seen during a typical day of treatment and the dramatic reduction in the need for hospital cases to treat high needs and uncooperative children.
In part three, I intend to explore how the introduction of SDF has impacted the number of dental procedures and the spectrum of procedures extending from prevention to surgical interventions over time.
During my dental training, I was taught to perform a comprehensive dental examination for new patients, and then craft a series of appointments to provide the appropriate clinical treatments. Over time, and as I became familiar with how the real world worked, it became obvious to me that many people postpone visiting the dentist unless they are experiencing some troubling symptoms. Hence, many initial appointments changed from comprehensive new-patient exams to limited problem-focused exams. Once the acute problem has been addressed, I always invite patients to return for a comprehensive examination. Unfortunately, many of these individuals fall back into the serial emergency-care-only category. The opportunity to treat all obvious dental decay with SDF at the initial visit should not be underestimated.
How I use SDF for caries treatment
The introduction of SDF into my practice enabled me to change my approach to caries treatment. Instead of waiting for a postexam appointment to start caries treatment, I can begin immediately during the exam appointment. It takes only minutes to treat many surfaces of active decay discovered during the exam.
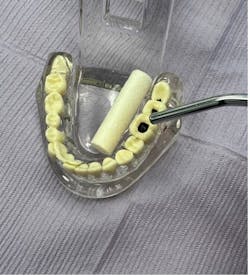
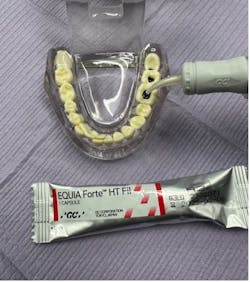
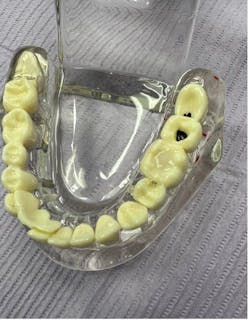
My technique is to carefully clean the lesion, dry it with compressed air, apply SDF with a microbrush, and then cover with fluoride varnish to prevent saliva contamination and diminish the strong taste of SDF. Depending on the size and location of lesions, it may be advisable to administer several treatments of SDF and fluoride varnish prior to determination of arrest. Following several days to weeks, the confirmation of success in arresting active caries is determined by the color of the lesion (black) and surface hardness to gentle probing.
A common follow-up procedure is to cover the arrested lesion with glass ionomer cement in order to restore lost tooth structure and to cover the dark arrested tooth structure with a tooth-colored material for esthetic reasons (figures 1–6). A common term used to describe this method of treatment is SMART (defined as silver-modified atraumatic restorative treatment).
Analysis of procedures before and after using SDF
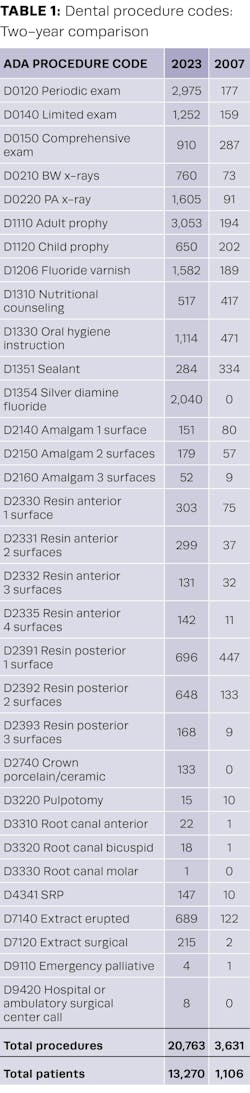
Rather than looking at a single day of treatment in 2007 and 2023 as I did in part two of this series, I created a scatterplot of selected procedures completed during these two years (table 1).
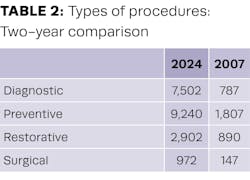
Let’s further organize this information into procedures that would be considered diagnostic, preventive, restorative, and surgical (table 2).
It is apparent that not only were far more people seen—13,270 versus 1,106 after implementation of SDF—but far more procedures were delivered—20,763 versus 3,631. I would attribute this to the more efficient manner in which our clinical resources have been made available to serve our community.
The integration of two methods of compensation—fee-for-service and capitation—has proven to be achievable, while at the same time providing successful disease management and a high level of quality restorative care.
Emergencies and after-hours calls
I would like to finish by mentioning another major change in our practice that has occurred over this time—emergencies and after-hours calls. Because there was no tracking by ADA code of emergency after-hours calls, it is more difficult to place a numerical quantification on this subject. My associate doctors and I recall that prior to the introduction of SDF into our practice, our after-hours pager was ringing every night and all weekend. Calling pharmacies, talking to ER departments, and occasionally coming into the office after hours was routine.
After 15 years of managing dental disease with SDF and intervening at an earlier stage in the disease, we have seen a dramatic reduction in emergency after-hours calls and the need to work emergencies into our regular patient schedule. My interpretation of this situation is that the level of acute disease in our community of patients has been diminished.
The integration of disease management tools (silver diamine fluoride) and minimally invasive technologies (glass ionomer cement) has allowed our Shoreview Dental clinic in Keizer, Oregon, to better serve our community of patients in numerous ways. We can identify dental disease earlier and begin treatment right away. These treatments often do not require the traditional tools of needles and drills, which many patients dislike. Our reputation as a “no fear and no pain” dental office has promoted dramatic practice growth during these 15 years. An additional benefit is to our clinical staff—SMART interventions are often low stress for our clinicians. One might label this experience as a triple win—for our patients, our staff, and the community.
Editor's note: This article appeared in the September 2024 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.