The effect of SDF on fee-for-service and capitation patient assignments
Editor's note: This is part two of a three-part series. Read part one here. Read part three here.
When I received my first bottle of Saforide, I let it sit on my desk for six months while I thought about what to do with it. Still, during this time, I continued to do the same things, such as hospital dentistry, sedations, and quadrant restorations.
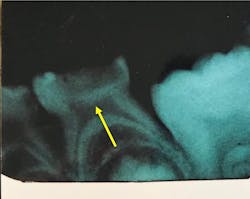
Since my waiting list for hospital dentistry cases was approaching six months and I was seeing abscesses occurring during the wait period, I decided to apply Saforide1 (figure 1) to lesions on the pending OR cases. My dental clinic is currently using the comparable product 38% silver diamine fluoride, Advantage Arrest, manufactured by Elevate Oral Care.
What happened when I applied Saforide
What I saw was astonishing! The abscesses stopped. The pain from active decay stopped. When we finally got into the hospital OR, it was clear that all lesions had become arrested, and that tertiary dentin was forming beneath arrested lesions (figure 2).
Finally, a tool was available to treat high-needs dental patients by stopping all decay in the mouth at once. Amazingly, this approach was also very inexpensive. A caries lesion could be treated with silver diamine fluoride (SDF) for about $1. The World Health Organization (WHO) recently added SDF to its list of essential medicines that should be available in every country.2
I began to treat all patients who had active decay using SDF at the initial exam appointment. A code to recognize this treatment was adopted by the American Dental Association in 2016—D1354. Another code, D1355, was created to consider SDF as a preventive agent.
The arrest of active caries does not eliminate the need for various forms of restorative care determined by the extent of damage caused by caries, and by patient preferences. In some cases where the primary tooth exfoliates, parents and patients have selected no further treatment. In other cases, various materials and methods have been chosen.
Some negatives of using SDF
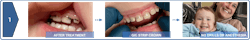
Side effects of treatment with SDF are a lesion color change to dark black and surface texture change from soft to hard. While this may not be a problem in a posterior occlusal groove, in the anterior region, the placement of a tooth-colored restoration will often be necessary for cosmetic reasons.
Figure 3 demonstrates the dark arrested caries after SDF application, followed by the placement of GIC strip crowns, with excellent esthetic results. Due to desensitization by SDF, this step can often be accomplished without local anesthesia. Interestingly, this color change may be used as a caries detector, as well as a treatment intended to arrest the lesion.
Same time spent on more patients
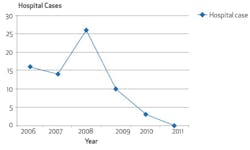
Another finding revealed from early intervention of all active lesions with SDF was a reduction in the number of after-hours emergency calls my practice received. Our patient base has grown dramatically between 2008 and 2023, and at the same time our after-hours emergency calls have dropped by 90%.
My need to take cases to the hospital for general anesthesia has plummeted.3 During a typical treatment day in the hospital, I could see, at the most, four patients. This reduction in hospital cases opened my schedule to see many more patients in the office (figure 4).
In a capitation reimbursement business model, the incentive is to have a large group of patients with few costly restorative needs whose oral health can be maintained. By adopting the combination of patient assignment with capitation, together with the low-cost treatment with SDF, I was able to open space in my schedule and accept a higher number of assigned patients. Our capitation assignment patient population has grown from 2,000 in 2008 to 5,000-plus today.
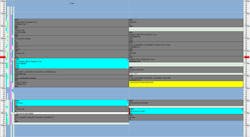
An example of this can be made by comparing my daily patient schedules from 2008 and 2023 (figure 5 and figure 6).
Over time, our fee-for-service practice component has grown and our capitation patient assignment has doubled. Many patients who began as assigned members chose to remain in the practice when their insurance changed to a fee-for-service model. This has required us to expand our office space and add clinical and support staff.
The fact that revenue is coming from multiple sources strengthens our business and improves overall profitability. We recently did an evaluation of the revenue, costs, and profitability in both the capitation and fee-for-service sides of our combined practice. We found that both models were equivalent from a straight business perspective. This was particularly evident during the recent pandemic when our office was essentially closed, but our large assignment population of healthy patients without active disease proved to be a vital asset.
See what the fee-for-service side of our practice looks like in Figure 7, and what does the capitation/Medicaid side of our office looks like in Figure 8.
A patient who enters our combined fee-for-service/capitation practice will see no difference between the two sides of the practice. The patient reception areas and clinical treatment rooms are identical. Our clinical staff are cross-trained to provide care in either the fee-for-service or capitation environment.
There’s nothing intrinsically good or bad about fee-for-service or capitation reimbursement models in dentistry. They can coexist in a practice that understands the fundamentals and incentives involved. When a dental practice is committed to ethically serving patients, they’ll encounter a wide range of clinical problems to solve and economic systems to support the appropriate interventions.
As a business owner, it’s also important to ensure that appropriate profitability is achieved through this process, to protect the interests of the clinical and support staff, and to update the clinic infrastructure.4 My experiences at Shoreview Dental LLC during the past 20 years have exceeded my expectations in service to our community and as a successful business financially.
During his 40 years of practice as a general dentist, Steve Duffin, DDS, worked in a rural solo practice with one employee, grew a large group practice with more than 20 locations, served as dental director and CEO of a large managed care DSO, and last, served as a primary investigator in large dental public health research programs. He’s currently the owner of Shoreview Dental LLC and dental director for the medical device manufacturer NoDK LLC.
Editor's note: This article appeared in the January 2024 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- National Center for Biotechnology Information. https://pubchem.ncbi.nlm.nih.gov/compound/Saforide
- CareQuest Institute commends WHO for adding three minimally invasive oral health care medicines. CareQuest Institute for Oral Health. October 6, 2021. https://www.carequest.org/about/press-release/carequest-institute-commends-who-adding-three-minimally-invasive-oral-health
- Duffin S. Back to the future: the medical management of caries introduction. J Calif Dent Assoc. 2012;40(11):853-858. doi:10.1080/19424396.2012.12224121
- Duffin S, Schwab J, Juhl J, Duffin M. SMART Oral Health: The Medical Management of Caries. Kindle Direct Publishing. 2019.