Decreasing open chair time through best practice management systems
This study of the financial loss of no-show appointments grew out of our two previous studies: “Economic impact of no-shows at the OUCOD student program”1 and “Impact of no-shows at OUCOD student program: Quality improvement study.”2 We determined that the University of Oklahoma College of Dentistry (OUCOD) had suffered significant financial revenue losses per academic year. Ultimately, we determined that no-show appointments negatively impact clinic time and production.
After manually inspecting clinic books, we found many no-show appointments excluded from the original no-show report. We continued to build on our initial guiding principle of “production lost today is production lost forever.” This study focused on decreasing open chair time through best practice management systems by sending electronic surveys to private practicing dentists across the US. It included multiple-choice and open-ended questions about management systems to reduce no-show appointments. Results were analyzed qualitatively and quantitatively. Responses from a total of 62 respondents were analyzed for this study.
Introduction
Effective practice management serves as the backbone that supports exceptional care and satisfied patients. When patients miss their dental appointments, it creates challenges, including financial strains for the dental office, missed opportunities to assist other patients in need, and increased number of dental emergencies for those who couldn’t make it to their appointments.
There is an opportunity for a practice to grow significantly by 30%-50% in production within the first three years; however, no-show appointments can slow this growth. To achieve success, it is recommended that a daily production goal be set.3 Dental practices must compensate for lost appointments with same-day appointments or other avenues to reach their daily production goals.3 If a dental practice were to sustain one no-show appointment per day for a year, the dental practice would exhibit a loss of $20,000-$70,000.4
Practice management encompasses strategic planning, financial management, and patient relationships. These elements work harmoniously to optimize the workflow, enhance patient experiences, and improve overall practice performance. With the growing complexity of dental health-care systems and technology advancements, practitioners face various challenges that require management to navigate effectively.
Implementing a communication system such as phone, email, mail, and text confirmations4 can combat potential revenue loss from no-show appointments. Reducing no-show rates can diminish costs and improve the quality of health-care delivery.5 This study aimed to determine the best practice management systems implemented within private practices to decrease open chair time.
Practice type distribution
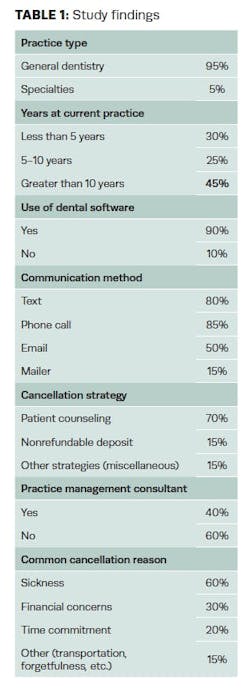
Ninety-five percent of respondents indicated that their practice type is general dentistry, with only 5% practicing in other specialties. This substantial percentage in general dentistry practices exhibits common challenges in managing patient flow, cancellations, and operational efficiency. General dentistry often involves recurring appointments, making it essential to ensure efficient management to minimize gaps in chair time. In contrast, specialty practices may reflect varying operational concerns, as specialties operate on a scheduled treatment timeline, reducing patient cancellations but requiring strict scheduling discipline.
Years at current practice
Regarding the respondents’ time at their current practice, 30% have been there for less than five years, 25% between five and 10 years, and 45% have over 10 years of experience. Respondents with over a decade of experience in their current practice suggest a tenured status, likely reflecting increased expertise in handling specific challenges regarding patient management.
Long-term practitioners may be more inclined to adapt cancellation strategies that resonate with their patient base due to the familiarity built over time. However, those under five years might still be figuring out operational practices or implementing strategies to gauge their effectiveness. Practitioners could be in a transitional phase between five to 10 years, assessing the results of prior strategies and possibly adopting sustainable management techniques.
Use of dental software
The data trend indicated a high rate of dental software usage for electronic health records, with 90% of respondents using dental software, while only 10% do not. This finding may highlight the dental industry’s direction toward digitization, which is increasingly recognized as essential for efficient patient management. Dental software organizes patient information and aids in appointment scheduling, automatic reminders, and analytics for better decision-making.
The 10% who do not use such software may represent smaller, older, or rural practices that may still rely on traditional, manual scheduling methods. However, the data trend suggests that digital tools are essential, especially since patients align with integrated technology environments. Using software allows for streamlined patient communications and record-keeping and reduces the likelihood of scheduling errors contributing to open chair time.
Communication methods
Regarding communication methods for reminding patients of their appointments, 85% of respondents use phone calls, followed by text messaging at 80%, 50% use email, and only 15% rely on mailers. Concluding from the data trend, there is a preference for direct and immediate communication methods in maintaining patient attendance.
While a time sink, phone calls offer a personalized touch that may appeal to patients and those requiring more detailed appointment information. Text messages, with their immediate delivery and broad accessibility, are appealing since they serve as a quick reminder. Emails provide an option for more detailed information, including preappointment instructions. However, the lower use of mailers reflects a decreasing reliance on traditional methods. Practices employing multiple communication methods enhance their outreach, minimizing the risk of cancellations due to forgetfulness or lack of timely reminders.
Cancellation strategies
The data trend revealed that 70% of respondents use patient counseling as a primary strategy to minimize cancellations. To effectively reduce no-show appointments, it is essential to counsel patients on the importance of attending appointments and informing them of the potential negative impacts of cancellations on their oral health and disease progression.
Additionally, 15% of practices use nonrefundable deposits as a deterrent, which is a more aggressive approach that may be more effective for specific patient segments or appointment types. Another 15% employ miscellaneous strategies, which include flexible scheduling, incentives for on-time attendance, or quick recalls to fill cancellations immediately.
These mixed strategies demonstrate that practices know the complexities behind patient cancellations and that a singular approach may not suit every patient demographic or practice style. For example, patient counseling works well for practices emphasizing patient relationships, while financial deterrents may be more effective for high-demand practices where open chair time is particularly costly.
Use of practice management consultant
Only 40% of respondents reported hiring a practice management consultant, while 60% have not. This split may reflect various factors, including the cost of consultancy, perceived self-sufficiency, or lack of familiarity with consultancy benefits. For newer practices or those struggling with high cancellation rates, consultants can provide an outside perspective and structured guidance on effective patient engagement and operational strategies. Consultants may help bridge knowledge gaps for practices looking to optimize chair time and establish efficient systems.
Common reasons for patient cancellations
The survey data indicated that 60% of cancellations are due to sickness, followed by financial concerns at 30% and time commitments at 20%. Transportation issues and forgetfulness were mentioned by 15% of the respondents. The data trend highlights the critical impact of external factors such as health and financial stability on patient appointment adherence. Practices may offer flexible rescheduling options for patients due to legitimate reasons for missing an appointment. Identifying these issues allows practices to develop targeted interventions.
Conclusion
The analysis revealed how respondents manage open chair time, enhance patient communication, and use technology for operational efficiency. Increased dental software use shows digital tools are key to practice management, aiding in scheduling, patient tracking, and reducing admin challenges. The varied communication methods highlighted the need for a multifaceted approach. Data on cancellations indicates that practices should focus on personalized patient engagement and that strong relationships can minimize no-show rates. Although rare, financial deterrents such as nonrefundable deposits can be effective when chair time is valued.
Understanding cancellation reasons stresses the necessity for empathy and flexibility in patient management, as cancellations often arise from issues beyond a patient’s control, such as illness or financial difficulties. The analysis helps practices align patient needs with operational efficiency, fostering strategies that address obstacles while mitigating the financial impact of no-shows.
Effective practice management is essential for patient retention, satisfaction, and operational efficiency. By promoting communication and follow-up, practices can strengthen patient loyalty and compliance, leading to better financial outcomes and improved oral health. As the dental field evolves, prioritizing effective management will be vital for delivering exceptional care.
Editor's note: This article appeared in the April 2025 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Elliott G, Kommareddi M. The economic impact of no-shows on dental practices. Dental Economics. July 5, 2023. https://www.dentaleconomics.com/practice/systems/article/14294871/how-the-economic-impact-of-no-shows-at-a-student-clinic-applies-to-dental-practices
- Kommareddi M, Elliott G, et al. Impact of no shows at OUCOD student program: quality improvement study. The University of Oklahoma College of Dentistry. April 25, 2024.
- Levin RP. Practice production, prioritized: reducing no-shows. Dental Economics. October 7, 2021. Accessed May 27, 2022. https://www.dentaleconomics.com/practice/article/14209915/practice-production-prioritized-reducing-noshows
- McGuire J. No more no-shows. Dental Economics. January 17, 2014. Accessed May 27, 2022. https://www.dentaleconomics.com/practice/article/16390417/no-more-noshows
- Levin RP. Practice production, prioritized: the impact of setting a daily goal. Dental Economics. May 27, 2022. Accessed May 27, 2022. https://www.dentaleconomics.com/practice/article/14270361/practice-production-prioritized-the-impact-of-setting-a-daily-goal