Each month, Dr. Gordon Christensen answers a question from our readers about everyday dentistry.
Q: I am a practitioner of 20 years, and I am seeing a trend evident among many practitioners in my area that is disturbing to me. It has always been my belief that, as dentists, one of our most significant professional responsibilities is to assist the public on how to keep their natural dentition for as long as possible—potentially for their entire lives. Yet, some practitioners are eager to accomplish root canals when teeth look even slightly questionable and remove teeth that could be easily restored. Amalgams that could serve for years are being removed only for esthetic reasons, taking away viable tooth structure and further weakening teeth. I am also seeing wanton removal of restorable teeth and unnecessary removal of bone to facilitate the placement of dental implants. Other colleagues have also commented to me on this current state of the profession. You are well known as a reputable dental speaker. What is causing these observable changes in the profession, and what can be done about our apparent shift in emphasis?
A: Unfortunately, your stated observations are correct. I am greatly concerned about the conditions you have described and many others. In my answer to you, I will state my own observations about the current state of the profession and how in our own practices we can help our patients better preserve their natural dentition for life.
There is an obvious movement toward measuring practice success by dollar production. This has happened because of numerous factors to move the profession toward business characteristics and away from professionalism. You don’t have to agree with my assessment. Let’s talk about some methods.
Adequate diet and oral hygiene throughout life
Teaching patients the importance of acceptable diet and oral hygiene throughout life is mandatory. However, all dentists and dental hygienists know well that in spite of our preaching, most patients fail miserably at both. What can we do about that?
Get patients on a routine schedule of dental hygiene appointments! It is near unbelievable that 70% of the adult American public sees a dentist at least once per year, which is unequaled in most countries. For those who have inadequate oral hygiene and diet, make sure that you have them using high-level fluoride-containing toothpastes, rinses, and perhaps fluoride-containing trays. Then, admit to yourself that, even with your best efforts, many patients will still have chronic dental caries and continuing periodontal disease.
More adequate evaluation of dental caries
Digital dental radiographs are inadequate in many ways. The thick, rigid CMOS sensors used by most practices in the US do not provide predictable identification, not only of initial caries but of large carious lesions as well. False positives and negatives abound when using the current generation of sensors. We need better sensors, but only manufacturers can help us with that problem. And it is long overdue!
So, get some help. Dexis CariVu (KaVo), Logicon Caries Detector Software (Carestream), Microlux Transilluminator (AdDent), and several other concepts can assist you in somewhat overcoming the faults of current dental radiography. Most of us are routinely missing caries and occasionally treating areas that do not have caries.Conservative restoration of teeth
Many dentists are still using large burs to cut initial carious lesions, such as no. 557 (figure 1). These are ancient designs with right-angle ends, crosscuts on the bur blades, and large diameters. They microscopically crack teeth and cut large preps that cause significant reduction in tooth strength. Use small burs like nos. 330, 329, 245, 1156 (figure 2) and others that have round ends and small diameters. Everybody wins: the patient has a stronger tooth, your procedures require less time, and you use fewer materials, which results in lower overhead costs.
Use of the best materials for specific situations
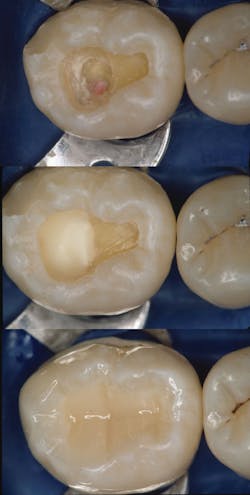
Composite resin is the most frequently used material in dentistry. It is excellent when used properly in small preps (figure 3). When used in large preps, the longevity of the restoration is greatly reduced, requiring replacement in a few years, removal of more tooth structure, and further weakening of the tooth. Although use of amalgam is controversial in some countries, it is still a viable option for large restorations in areas that do not require esthetic acceptability. The longevity of amalgam is well researched and up to twice that of composite, therebyWhen treating patients with high caries activity, the newer forms of conventional glass ionomer should be used either as the complete restorative material in small preps or as a replacement for dentin in larger preps. Equia Forte or Equia Forte HT (GC America), Ketac Universal (3M), and other newly introduced brands are improved glass ionomers that release significant amounts of fluoride and lengthen the time until the restorations need to be redone.
Using crowns conservatively
Unless required for esthetics or because of significant tooth structure destruction, crowns should be the last restorative option. Crowns remove nearly all of the enamel and usually leave only the already-destroyed central portion of the tooth. Even though I am a prosthodontist specializing in dentitions that are mostly destroyed, I still feel that crowns are used far too frequently.
Keeping occlusion healthy
Unfortunately, many dentists nearly forget occlusion. Accomplishing restorative dental procedures and not adjusting occlusion properly often promotes open contacts, broken restorations, and overall degeneration of the dentition (figure 3). This point is especially true due to the increasing use of implants and the fact that they move only slightly in the bone, while teeth move constantly and significantly in the bone, thus heavily influencing occlusal breakdown.
Using root canal treatment only when needed
Properly accomplished root canal treatment is a necessary technique, but I am seeing some practitioners move too rapidly to devitalize teeth and perform root canals. Current pulp capping procedures—indirect (no pulp exposure) and direct (pulp exposure)—should be used more often, reducing the need for root canal treatment. The following characteristics should be present for successful pulp capping (figure 4):
• Healthy patient, preferably with apparent tooth vitality present according to testing
• No pulp exposure or a small (0.5 mm to 0.75 mm) exposure
• If pulp exposure, there is slight red blood exuding—not magenta, not serous, not purulent
• Use of popular, proven pulp capping materials—examples are Vitrebond Plus (3M), Fuji Lining LC (GC America), MTA pastes from Ultradent, Dentsply, Avalon, and others—accompanied by informed consent for the patient about expectations of the indirect or direct pulp cap
Using implants should be the last resort
In the US, we are in ethical trouble with this concept! Many of us have seen patients who have had teeth removed that could have easily been restored or didn’t even need restoration, only to allow implants to be placed. Patients have been provided with various reasons for the removal of teeth, some legitimate and others approaching malpractice. The result is dependence on the viability of implants, many of which are being observed with various levels of peri-implant mucositis or peri-implantitis after only a few years. Having placed and restored implants for more than 30 years, I contend that patients should be provided with treatment plans that include keeping their teeth as well as implant options. Implants are a wonderful alternative when needed, but they should be considered as the last resort.
Summary
Your patients are living until about 80 years of age. Natural teeth that have had proper nutrition, ongoing dental hygiene care, minimal oral restorative treatment, and lack of occlusal bruxing habits can last that long. Oral conditions, as with overall body characteristics, break down and degenerate as we age. Accelerating the breakdown of the dentition with prematurely large restorations, crowns, root canal treatment, extraction, and implant placement leads only to premature breakdown of overall oral and systemic health (figure 5).
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic for you and your staff.
One-hour videos:
Diagnosis and Treatment of Failing Implants (Item V2391)
Making Foolproof Class II Restorations (Item V3501)
Foolproof, Fast, Single-Crown Procedure (Item V1980)
Two-day hands-on courses:
Implant Surgery—Level 2 with Dr. Gordon Christensen
Restorative Dentistry 2—Fixed Prosthodontics with Dr. Gordon Christensen
For more information about these educational products, call (800) 223-6569 or visit pccdental.com.
Gordon J. Christensen, DDS, PhD, MSD, is a practicing prosthodontist in Provo, Utah. He is the founder and CEO of Practical Clinical Courses, an international continuing education organization founded in 1981 for dental professionals. Dr. Christensen is cofounder (with his wife, Rella Christensen, PhD, RDH) and CEO of Clinicians Report.