Jungyi Alexis Liu, DDS, MS
Kevin J. Donly, DDS, MS
There have been great strides in reducing the incidence of dental disease during the past seven decades. However, dental caries remains a prevalent disease in children, with 75% of United States children experiencing dental caries by age 17.1
The use of fluoridated dentifrice, fluoridated mouth rinses, the initiation of community water fluoridation, campaigns to educate the public on the prevention of dental disease, and professionally applied fluorides have all been good efforts to prevent dental disease. Yet Third National Health and Nutrition Examination Survey (NHANES III) data reported an increase in dental caries prevalence in two- to five-year-old children.1 In fact, the caries experience data from 2011 to 2014 indicated 23.8% of preschool children still have dental caries. The first Surgeon General’s Report on Oral Health (2000) indicated that the populations most affected were Hispanic and African American.2
Due to the increase in caries in these very young children, particularly uninsured children, alternatives to traditional restorative dentistry were considered. Many of the very young children did not have the level of behavior development to be able to cooperate for traditional restorative dentistry. Likewise, the practicality of providing care in a hospital setting was difficult due to operating room availability and relatively high cost. The expense of treating children who are underserved and uninsured creates cost barriers, so alternative care became increasingly necessary.3
Silver diamine fluoride
Silver nitrate and silver diamine fluoride (SDF) have been utilized in other countries as a way to arrest caries progression.4 Silver particles penetrate the surface of caries-infected tooth structure to create a barrier, presumably as silver phosphate, and the fluoride is most likely deposited on tooth structure as calcium fluoride with some fluoride being integrated within hydroxyapatite to form fluorapatite and/or fluoridated hydroxyapatite.5 As we know, heavy metals have antimicrobial properties, as do high doses of fluoride. Studies have indicated the effectiveness of SDF to arrest the progression of dental caries.6–9 It has been shown that the clinical application of SDF twice is almost three times more effective at arresting the progression of dental caries than a single application of SDF.10,11 There is also evidence that active caries does not need to be completely removed prior to SDF application for the SDF to be effective for dental caries arrest.7 Food debris should be removed from the cavity to provide the maximum contact of SDF with caries-affected dentin. SDF was approved by the United States Food and Drug Administration in 2014 as a product to reduce tooth sensitivity, similar to sodium fluoride varnish. Many dentists are using SDF off-label as a professionally accepted way to arrest the progression of dental caries.12,13
There are important considerations that are necessary when SDF application may be recommended. We consider SDF application to be a restorative dentistry procedure, as active caries is treated and the treatment is not reversible. The procedure code for applying SDF is D1354 as interim caries arresting medicament application. Reimbursement for this procedure varies among states and insurance companies. Most importantly, SDF provides a less invasive and an inexpensive approach for managing caries. However, SDF is not a prevention measure and cannot replace the use of fluoride varnish in preventing caries.The main disadvantage of SDF is the permanent discoloration of the enamel and dentin of the lesion. If SDF is in contact with skin, it creates temporary staining and will disappear in two to 14 days after natural exfoliation of the skin.14 SDF will darken tooth structure, so it is very important that parents understand this fact. The American Academy of Pediatric Dentistry recommends that informed consent be obtained from parents prior to SDF application.13,15 The saying “a picture is worth a thousand words” seems appropriate in these circumstances, where SDF will turn infected tooth structure black (figures 1 and 2). Be sure parents and caregivers are well aware of the staining associated with SDF. Additionally, SDF can also permanently stain clinical operatory surfaces and clothes.
Applying potassium iodide immediately after SDF can decrease the discoloration of the caries lesion.14 When potassium iodide is in contact with SDF, excess silver ions causing black stains from SDF are removed by forming a silver iodide precipitate. Riva Star is a new product from SDI Limited that assists with this process. Riva Star uses a two-step procedure with SDF followed by application of potassium iodide. Riva Star is advertised to reduce staining and be esthetically pleasing to patients.16Teeth exhibiting pulpal involvement are not candidates for SDF treatment.3 A thorough diagnosis is necessary because SDF is to be used to arrest caries on vital teeth and is not indicated for use on nonvital teeth. If an SDF-treated tooth needs to be restored, SDF does not affect bonding strength of resin-based composite to dentin using either self-etch or full-etch systems.17,18
Another factor that is important is the safety of SDF. A typical application of SDF to an erupted primary dentition is approximately 0.05 ml. Although there may be variations in the exact amount of silver and fluoride as the SDF solution ages, the amount of silver and fluoride still falls well within a safe level.19,20
Clinical procedure of SDF application
The following is a step-by-step method for applying SDF:
• Use a plastic-lined bib to cover the counter to prevent staining. Protect patients with a plastic-lined bib and glasses.
• Remove gross debris from the cavitation. Excavation of dentinal caries is not necessary (figure 1).
• The placement of orthodontic separators prior to the procedure may be helpful to access interproximal caries lesions.
• Minimize SDF contact with gingiva and mucous membranes. Consider applying a protective coating (e.g., cocoa butter or petroleum jelly) limited to the gingiva and lips.
• For the tooth that is to receive SDF, isolate with gauze, cotton rolls, or other methods.
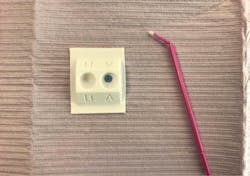
• No more than one drop of SDF in a plastic dappen dish is necessary (figure 3). SDF corrodes glass and metal.
• Dry the lesion with compressed air before SDF application. If this is not possible, dry with cotton rolls or gauze.
• Bend a micro sponge brush before dipping it into SDF. There is a blue-tinted SDF available to make it easier to see where the SDF is placed (Advantage Arrest, Elevate Oral Care). Remove the excess liquid by dabbing the brush on the side of the dappen dish. Directly apply SDF only to the surface of tooth structure exhibiting caries (figure 4).
• Dry with gentle air for at least one minute. Remove excess SDF with gauze or a cotton roll. If possible, continue the isolation for up to three minutes.
• Ideally, application time should be one minute with a flow of air to dry the SDF liquid. This can be difficult in very young patients due to lack of cooperation. If application time is shorter, carefully monitor at the follow-up visit to reassess the need for SDF reapplication.
• There are no specific restrictions following treatment.
• Timing for follow-up: If possible, follow-up on the caries arrest can be scheduled two to four weeks after SDF application.13 Consider reapplication of SDF if the lesion is not hard or dark. The follow-up schedule can be based on the patient’s caries risk and caries progression.
Conclusion
In summary, SDF offers another option to treat caries, at least intermediately. Arresting caries, particularly in very young children who may be precooperative, can be effectively integrated into any dental practice. SDF is safe and effective but does discolor teeth. Risks and benefits can be discussed with parents, and an agreement can be reached on what is best for the child patient.
References
1. Centers for Disease Control and Prevention, National Center for Health Statistics. Third National Health and Examination Survey Data. (NHANES III). Hyattsville, MD: U.S. Department of Health and Human Services, Center for Disease Control, 2012. Available at https://www.cdc.gov/nchs/nhanes/nhanes3.htm. Accessed March 22, 2017. Archived by WebCite at http://www.webcitation.org/6p9cTnaGZ.
2. Oral health in America: a report of the Surgeon General. J Calif Dent Assoc. 2000;28(9):685-695.
3. Crystal YO, Niederman R. Silver Diamine Fluoride Treatment Considerations in Children’s Caries Management. Pediatr Dent. 2016;38(7):466-471.
4. Rosenblatt A, Stamford TC, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet”. J Dent Res. 2009;88(2):116-125.
5. Zhao IS, Gao SS, Hiraishi N, et al. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Int Dent J. 2018;68(2):67-76.
6. Gao SS, Zhao IS, Hiraishi N, et al. Clinical Trials of Silver Diamine Fluoride in Arresting Caries among Children: A Systematic Review. JDR Clin Trans Res. 2016;1(3):201-210.
7. Chu CH, Lo EC, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81(11):767-770.
8. Llodra JC, Rodriguez A, Ferrer B, Menardia V, Ramos T, Morato M. Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res. 2005;84(8):721-724.
9. Yee R, Holmgren C, Mulder J, Lama D, Walker D, van Palenstein Helderman W. Efficacy of silver diamine fluoride for Arresting Caries Treatment. J Dent Res. 2009;88(7):644-647.
10. Zhi QH, Lo EC, Lin HC. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J Dent. 2012;40(11):962-967.
11. Fung MHT, Duangthip D, Wong MCM, Lo ECM, Chu CH. Arresting Dentine Caries with Different Concentration and Periodicity of Silver Diamine Fluoride. JDR Clin Trans Res. 2016;1(2):143-152.
12. Crystal YO, Marghalani AA, Ureles SD, et al. Use of Silver Diamine Fluoride for Dental Caries Management in Children and Adolescents, Including Those with Special Health Care Needs. Pediatr Dent. 2017;39(5):135-145.
13. American Academy of Pediatric Dentistry. Policy on the Use of Silver Diamine Fluoride for Pediatric Dental Patients. Pediatr Dent. 2018;40(6):51-54.
14. Horst JA, Ellenikiotis, H., Milgrom, PL. UCSF Protocol for Caries Arrest Using Silver Diamine Fluoride: Rationale, Indications and Consent. J Calif Dent Assoc. 2016;44(1):16-28.
15. American Academy of Pediatric Dentistry. Chairside Guide: Silver Diamine Fluoride in the Management of Dental Caries Lesions. Pediatr Dent. 2018;40(6):492-493.
16. Riva Star is a new generation desensitizer which immediately removes tooth sensitivity. SDI Limited website. https://www.sdi.com.au/au/en-us/product/rivastar/?fbclid=IwAR2JlITf2OR6U-jR2YQhh0—2hYTI_wk6gVJ0lRqA_zUdGUNukxM44ytWU0. Accessed April 15, 2019.
17. Quock RL, Barros JA, Yang SW, Patel SA. Effect of silver diamine fluoride on microtensile bond strength to dentin. Oper Dent. 2012;37(6):610-616.
18. Selvaraj K, Sampath V, Sujatha V, Mahalaxmi S. Evaluation of microshear bond strength and nanoleakage of etch-and-rinse and self-etch adhesives to dentin pretreated with silver diamine fluoride/potassium iodide: An in vitro study. Indian J Dent Res. 2016;27(4):421-425.
19. Crystal YO, Rabieh S, Janal MN, Rasamimari S, Bromage TG. Silver and fluoride content and short-term stability of 38% silver diamine fluoride. J Am Dent Assoc. 2019;150(2):140-146.
20. Lin YS, Rothen ML, Milgrom P. Pharmacokinetics of 38% topical silver diamine fluoride in healthy adult volunteers. J Am Dent Assoc. 2019;150(3):186-192.
JUNGYI ALEXIS LIU, DDS, MS, is an assistant professor in department of developmental dentistry at the University of Texas Health San Antonio School of Dentistry.
KEVIN J. DONLY, DDS, MS, is the president of the American Academy of Pediatric Dentistry. He is a professor and chair of the department of developmental dentistry at the University of Texas Health San Antonio School of Dentistry.