As dental professionals, we play an important role in our patients’ overall health. We have the ability not only to educate them on proper oral hygiene and heal them from diseases, such as periodontitis and dental caries, but we also have the opportunity to touch their lives in ways no other health-care professional does. Dental professionals are the ideal health-care providers to perform a thorough head, neck, and intraoral exam. Oral cancer screening is among the most important services we offer our patients, because it could be the difference between life or death.
Oral cancer prevalence
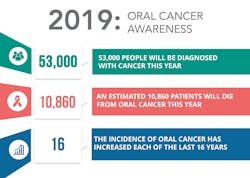
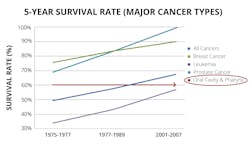
The incidence of oral cancer has increased each of the last 16 years. Since 2011, the number of people diagnosed with oral cancer has more than doubled, and in 2019 alone, it is estimated that a total of 53,000 people will be diagnosed with oral cancer (figure 1).1 Regarding survival rates, oral cancer is one of few major cancers that has not changed its five-year survival rate in decades (figure 2). More incidences of oral cancer are resulting in late-stage discovery.
The conventional oral examination (COE), a visual method, relies heavily on the clinician’s expertise and keen eye to detect neoplastic changes that suggest symptomatic alterations of the mucosal surface. Now, with the latest technologies in our dental practices, we can utilize an adjunct screening device to aid us in changing the trends of oral cancer by allowing us to discover mucosal abnormalities at their earliest stages. Saini et al. concluded in a recent study evaluating the efficacy of fluorescence technology versus COE that OralID (Forward Science) is a true adjunct to COE in the visualization of potential malignant changes.2
Malignancies found at late stages account for 71% of diagnosed oral cancers and are unfortunate due in part to increased morbidity rates. However, this statistic also emphasizes the importance of oral cancer screening and early detection, because when discovered early, these cases have a survival rate between 80% and 90%.1
Early discovery saves lives
For many years, incorporating advanced technology has provided clinicians with the ability to offer a higher quality of care for their patients. Pap smears, colonoscopies, PSA tests, and mammograms have all given clinicians the opportunity to discover cancer at its earliest stages to save more lives. Oral cancer is no different, and oral cancer screening in the dental office can save lives. Here are a few stories of clinical lifesavers to further exemplify the importance of the early discovery of oral cancer.
Lifesaver No. 1
One day, Robert Burnett, DDS, a general practice dentist in Tyler, Texas, and fellow of the Academy of General Dentistry, detected a suspicious-looking lesion under the right side of a patient’s tongue using OralID. He initially performed a liquid-based cytology, CytID (Forward Science), which came back suggesting a reactive atypia or neoplasm. His team then sent the patient to an oral surgeon for a more extensive biopsy.
The results revealed a squamous cell carcinoma, slightly invasive to the surrounding muscle. The patient chose to go to MD Anderson Cancer Center in Houston, Texas, to have the lesion excised. Fortunately, they were able to get it excised before the lesion grew larger or metastasized to other areas. No radiation or chemotherapy was needed.
Lifesaver No. 2
Kristin Utley, a registered dental hygienist in Colorado, had a male patient in his late 50s who was trying to quit smoking. He sucked on lemon drops and chewed Juicy Fruit gum all day to fight his nicotine cravings. Because of the lemon drops, his tissues were always inflamed, plus he was battling moderate to severe periodontal disease and recurrent decay from the gum. Utley found what appeared to be a lesion from the patient’s lemon drop habit on the left lateral border of his tongue adjacent to tooth No. 17. Upon examination with OralID, it was determined that the patient indeed had a lesion. After a two-week follow-up, the lesion still exhibited a loss of fluorescence, so the patient was referred to an oral surgeon for biopsy.
The results came back as severe dysplasia. The oral surgeon believed that if the patient had waited another year to be examined, he probably would have needed a neck dissection and radiation. The patient was able to have the lesion removed by excision and now has a detailed oral cancer exam at every dental visit due to his risk profile.
Lifesaver No. 3
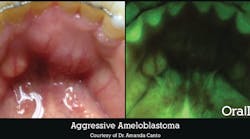
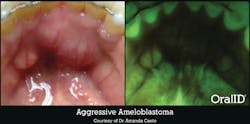
Not every lesion we find ends up being malignant, but it could still be something that causes our patient harm. Amanda Canto, DDS, owns a practice in Houston, Texas, with a cosmetic dentistry focus. One day, she was performing her routine, conventional oral exam on a 49-year-old retired nurse. The patient appeared to have multiple mandibular tori, lingual to her mandibular anteriors. OralID fluorescence examination revealed a very large area that exhibited a loss of fluorescence or darkness. Dr. Canto was immediately concerned and sent the patient for a biopsy.
The results revealed that there was an aggressive ameloblastoma (figure 3), which is a benign tumor. The problem with this type of tumor is that it will continue to grow, causing extreme disfigurement, if all of the cells are not resected. Unfortunately, in order to remove all of this tumor and keep it from growing, the patient had to have a portion of her jaw resected in a surgery very similar to what many oral cancer patients experience. When performing an oral cancer exam, we’re not just looking for cancer; we’re looking for anything abnormal. This particular lesion still turned out to be life-changing for the patient.
Conclusion
Oral cancer has been on the rise for decades, calling for us to make it a priority to enhance the standard of care for our patients. Our profession has the opportunity to utilize advanced technology and truly save lives. So, when your next patient sits in the chair, ask yourself this: If your patient were a loved one, would you be secure enough in the technology you are currently using?
References
1. American Cancer Society. Cancer Facts & Figures 2019. Atlanta: American Cancer Society; 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf.
2. Saini R, Cantore S, Saini SR, Mastrangelo F, Ballini A, Santacroce L. Efficacy of fluorescence technology vs conventional oral examination for the early detection of oral pre-malignant lesions. A clinical comparative study. Endocr Metab Immune Disord Drug Targets. 2019;19(6):852. doi:10.2174/1871530319666190119103255.