Joshua P. Weintraub, DDS
Technology continues to expand the scope of general dentistry, and dental lasers are at the forefront of bridging the multidisciplinary gap. Throughout my career, I have worked with a variety of laser systems at different wavelengths, including erbium (2.9 μm), Nd:YAG (1.064 μm), and diode (0.81 μm). While effective, I needed more from the devices. I needed a laser that could reliably perform anesthesia- and blood-free procedures for the majority of my cases.
The introduction of Convergent Dental's CO2 laser, Solea, met that requirement. The Solea laser uses a 9.3 μm wavelength to cleanly vaporize hard, soft, and osseous tissues. It also allows general dentists to both confidently and safely perform procedures traditionally reserved for specialists. Solea similarly adds value to the specialty practice, where patients can experience a virtually pain-free and often suture-free procedure in half the amount of time.
READ MORE |4 reasons you need a dental laser in your practice
To better explore how this laser has broadened my surgical repertoire, I will discuss two crown-lengthening cases. Before a tooth can be permanently restored, crown lengthening may be a necessary part of the treatment plan. In other cases, it can also deliver optimal esthetics and eliminate a patient's "gummy smile" or even out gingival margins to optimal levels. While this procedure can appear intimidating or time-consuming to a general practitioner, Solea promises simplicity and greater ease of use. The majority of procedures can be managed with its one "Hard and Soft Tissue" setting. And, with the laser's variable-speed foot pedal, one simply presses harder on the pedal for harder tissue and softer for softer tissue. This allows the doctor to focus on the patient and oral cavity.
Computer-controlled motors, called galvos, move mirrors inside the handpiece that project spot sizes of various diameters, 0.25 mm to 1.25 mm. This computer technology ensures the appropriate width of incision at the surgical site as directed by the doctor. With these features, excellent results are achieved with the laser, and procedures are completed with minimal bleeding and faster healing. Patients experience significantly reduced postoperative pain. I am always amazed that my patients report such minimal discomfort when I make my follow-up phone calls the evening after procedures.
As I mentioned, Solea is reliably anesthesia-free for the majority of hard- and soft-tissue procedures, but for the two crown-lengthening cases I will describe, local anesthetic was used. I typically use local anesthetic for deep, invasive procedures and those that involve bone. Even with the use of local anesthetic, benefits are realized through precise ablation, clean soft-tissue cutting, and faster healing times (with minimally invasive procedures).
Clinical case 1: Flapless esthetic crown lengthening
This procedure includes the removal of both soft tissue and bone, using Solea's Ultraguide handpiece. It demonstrates precision, clean cutting, and very fast healing. Closed/flapless crown-lengthening procedures with lasers can be controversial, and for good reason. Complete understanding of proper bony architecture is imperative. Removing osseous tissue from only the facial or lingual will not compromise ideal architecture. However, removing interproximal bone without a flap is contraindicated as iatrogenic osseous/periodontal defects will be created.
This patient came directly out of hygiene with a chipped tooth. The patient was aware that teeth Nos. 7-10 were in need of crowns. Tooth No. 8 was bonded (figure 1). The patient was informed that this was a temporary fix and agreed to schedule crowns for teeth Nos. 8 and 9. Due to wear, secondary to bruxism, teeth Nos. 8 and 9 had supererupted, bringing their gingival margins too far coronal for proper esthetics. A preprosthetic esthetic crown lengthening was suggested to ensure optimal esthetics. Orthodontic intrusion was also considered, but the patient was not interested. A mock-up of the results in gingival margin improvement was demonstrated with flowable composite. The patient preferred this option to surgery with a periodontist, which would have included a flap and four to six sutures. Soft tissue and approximately 2 mm of bone needed to be removed in order to reestablish proper gingival levels. This was an unscheduled case; the patient came right out of hygiene and requested to complete the crown lengthening procedure while she was in the office. She just wanted to be sure that it was still okay to meet her friend for lunch (it was, and she had sesame chicken).
Figure 1: Pre-op
Figure 2: Immediate post-op
Figure 3: Seven-days post-op
Figure 4: 30-days post-op
Figure 5: Complete with e.max crowns
The patient was anesthetized with 1 carpule of 4% articaine with epinephrine 1:100,000. The entire procedure was performed using Solea's "Hard and Soft Tissue" setting. Excess gingiva was removed using the Solea Ultraguide handpiece with a 600-micron tip, 14 mm length, and the 0.25 mm spot size. One percent mist and cutting speed between 20% and 40% were selected. The bone adjacent to the tooth was removed until the proper gingival architecture was achieved with the corresponding bony architecture 3 mm apical to the desired gingival margins. This was accomplished using the same Ultraguide tip, 0.25 mm spot size, 100% mist, and cutting speed between 40% and 60%. Full mist is always used with bone. A piezo scaler was used to smooth the root surface and remove any spicules of bone on cementum. The total procedure time was approximately 40 minutes (figure 2). The patient was reevaluated at seven days (figure 3) and 30 days (figure 4). Preparation and impressions for IPS e.max (Ivoclar Vivadent) crowns for teeth No. 8 and 9 were completed after three weeks, and final crowns were inserted (figure 5).
Solea's precision and ability to maintain a clean surgical site allowed this unscheduled procedure to be completed successfully. Additionally, rapid healing was observed (figure 3). With Solea, this was a minimally invasive procedure and crowns were prepared 30 days postoperatively (figure 5). Traditional surgery would require six to eight weeks until proper conditions were established for definitive restorative work. In addition, there would have been more postoperative pain and slower healing with traditional instruments.
READ MORE | Shining the light on laser safety: 4 steps to keep your practice compliant
Clinical case 2: Open crown lengthening
This procedure involved ablation of both soft tissue and bone with minimal bleeding and minimal postoperative discomfort with rapid healing.
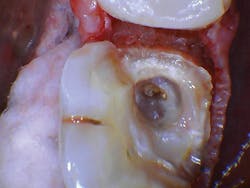
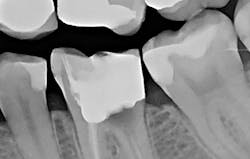
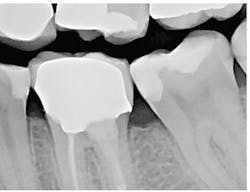
The patient presented with tooth No.19 ML with a history of endodontic treatment fractured to the level of the alveolus (figures 6-8). The patient had an inadequate clinical crown to restore. The options were either to extract the tooth and place an implant, or complete a crown lengthening and then restore. The clinical objective of crown lengthening was to establish biologic width and expose enough tooth structure coronal to the bone for a proper restoration. The patient opted for crown lengthening, and the procedure was completed in about 50 minutes.
Figure 6: Pre-op
Figure 7: Pre-op
Figure 8: Pre-op
The patient was anesthetized with 1.7 ml of 4% articaine with epinephrine 1:100,000. The entire procedure was performed using the "Hard and Soft Tissue" setting. The gingiva was flapped to expose bone using the 0.25 mm spot size with 1% mist and cutting speed between 20% and 50% (figures 9-10). Only 0.5 mm of tooth structure was coronal to the alveolar bone. The osseous tissue was removed to establish biologic width and expose tooth structure coronal to bone for a proper restoration (figure 11). Proper positive bony architecture was maintained. The 0.75 mm spot size was used with 100% mist and cutting speed between 30% and 60%. A temporary restoration was placed, followed by one suture (figure 12). The total procedure time was 50 minutes. The patient was reevaluated after seven days (figure 13), and the final crown was placed (figure 14).
With traditional instruments, this procedure is typically completed with a scalpel and high-speed handpiece with burs. A larger flap is required to improve visibility and instrumentation. However, with Solea's precision and small spot-size options, a much smaller flap was needed. There was less bleeding, resulting in a cleaner surgical site and faster postoperative healing. As the radiograph and photos show, excellent conditions for the final restoration were established. The final crown demonstrated sound margins and evidence of proper biologic width. As the five-day follow-up photo shows, the healing time was fast, and tissues appear healthy.
Figure 9: Initial incision
Figure 10: Initial incision
Figure 11: Flapped, postosseous reduction
Figure 12: Immediate post-op
Figure 13: Seven-day follow-upCrown lengthening
Figure 14: Crown inserted
It is clear that Solea enhances the dental experience for both the provider and patient. The precision of the computer-controlled, CO2 laser ensures a clean, virtually blood-free working site before, during, and after surgery. Solea's unique ability to vaporize all tissue in the oral cavity translates to improved clinical performance and patient experience. Without the intimidating noise of a high-speed handpiece, my patients actually enjoy their dental visit and are consistently amazed at the lack of significant postoperative discomfort. The technology also enables me to expand the services I offer to patients, which improves their experience because I am able to perform their surgery instead of having to refer them to a specialist.
Although the two cases here used local anesthetic, more than 95% of my hard- and soft-tissue procedures are completed anesthesia-free. In fact, I am so confident that I can perform minimally invasive dentistry reliably anesthesia-free-with the exception of some procedures such as flapped surgery-that I don't hesitate to perform procedures the same day the need arises. Patients really appreciate the convenience. I am confident that this breakthrough technology can expand services to your patients, and Solea is well within the cost reach of any general dentist.
Joshua P. Weintraub, DDS, is a 1996 graduate of the University of Maryland Dental School. He began his dental career in the US Navy Dental Corps as a lieutenant in Okinawa, Japan, followed by the Navy Yard in Washington, DC. He entered private practice in 1999 and has used dental lasers since 2008, including erbium and Nd:YAG. He currently uses a CO2 9.3 μm laser (Solea, Convergent Dental) in his practice. Dr. Weintraub is an international lecturer.