Each month, Dr. Gordon Christensen answers a question from readers about everyday dentistry.
[Q] Your organization has been evaluating dental products for many years. I have been practicing for about 10 years, and I am not seeing much change in numerous dental product types that obviously need improvement. What is holding back improvement? In your opinion, what are the dental product categories that really need change, and how can we practitioners stimulate that change?
[A] I agree completely! Routinely, I see various dental products of all types that need improvement. Why do these needed improvements not happen faster and more thoroughly? There are many reasons, and I will mention only a few obvious ones. Dental manufacturers large and small have similar challenges. They are spending time, energy, and financial resources on keeping up with their current product needs and improving them minimally, using their already-present patents and FDA clearances. They are keeping their companies financially stable. Spending time and money on developing new concepts requires employees, money, and time away from their current product lines. The result is the needed improvements are not implemented until the market demands change.
You’ve asked me to identify some product areas in need of improvement, and I will include my opinion of the most important ones. I consider them crucial because general dentists use these concepts every practice day, and millions of patients suffer because of the concept or procedure inadequacies. The following areas are only a few of those needing improvement. I will provide my personal observations on what needs to be done to each.
Composite restorations
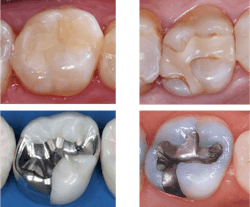
General dentists place numerous composites every day. The clinical longevity of composites is well known to be far shorter than that of amalgam restorations (figure 1). Several reasons relate to their short lifespan, including 2% shrinkage producing microscopically open margins on all restorations, no cariostatic activity provided by composite materials, inadequate curing accomplished by many dentists, occlusal wear, and other issues.
Since composite restorations are the most-used dental restoration type, and their inadequacies are obvious, this topic should be the highest priority for companies producing these products and for government agencies funding research. Our patients need nonshrinking, cariostatic, esthetic materials providing long-term service immediately!
Digital radiographic sensors
Ask any mature dentist familiar with analog radiography of the past, and they will tell you about their dissatisfaction with most digital radiographic sensors when compared with analog radiographic images. What are some of the challenges?
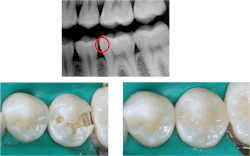
The digital images show only about 50% of the actual depth of small lesions. This often delays tooth restoration, causing unnecessary challenges with greater tooth destruction, more time and material used, wider exposure of restorations to occlusal wear, and potential pulpal damage (figure 2).
Sensors are about 9 mm thick and rigid. They cannot be adapted to the dental arch curvature, and they provide unequal radiation to the teeth and inaccurate identification of caries.
The cost of digital sensors is high and unjustified in the opinions of many dentists. Just like composites mentioned previously, dentists take radiographs many times per day. The manufacturer who overcomes these challenges will rapidly dominate the radiographic market. It is time for manufacturers to improve these inadequate diagnostic issues.
Zirconia restoration refinement
It is well-known that patients need fixed prosthodontic procedures routinely, and they contribute heavily to the overall gross income of dental practitioners. The zirconia revolution of the past nearly 20 years has shown zirconia to be the most-used material for crowns and fixed prostheses. Although zirconia has the potential to provide excellent restorative services, there are a few aspects of the lab and clinical procedures that need significant change. These are only some of the issues.
It has been estimated by labs that 40%–50% of impressions currently sent to labs are scanned by dentists (personal communication, Glidewell Laboratories, January 2025). Other dentists are sending vinyl polysiloxane or polyether impressions to labs, and the lab personnel are scanning the impressions. Another few dentists are sending poured casts to the labs, and the lab personnel scan the casts. The result is that almost all impressions for crowns and fixed prostheses are scanned. Isn’t that good? It’s good for labs because it reduces time to produce the restorations. But the accuracy of scanners needs significant improvement! It does not come close to the accuracy of elastomer materials. This issue is well-known by manufacturers, and they are working with AI and other factors to improve it. Dentists need accurate, inexpensive, small scanners immediately.
Cariostatic cements. Because of the scanner inaccuracies, milling devices, the ceramic pressing concept, and other issues, the margins of zirconia and lithium disilicate crowns are significantly more open than the metal restorations of the past. Resin-modified glass ionomer (RMGI) and conventional glass ionomer (GI) cements are cariostatic, but resin cements are composite and have the same characteristics as described previously for composite. Do we want these open margins and shrinking cements to cause caries on margins in a few years?
Historically, with a few exceptions, crowns did not come off in service. Zinc phosphate and conventional GI cements are rigid and strong and held the crowns on the tooth preparations. Resin cements are flexible and strong (figure 3). But one of the major reasons almost every dentist has had zirconia crowns coming off is the flexibility of resin cements and, to a lesser degree, the flexibility of the RMGI cements (figure 4).
Dentists need rigid, strong, cariostatic cements almost every day of practice. As with composite restorative materials, resin cements need cariostatic properties immediately! In the interim, until resin cements are modified, I suggest that dentists should use RMGI and GI cements for crowns and fixed prostheses.
Implants
Dental root-form titanium alloy implants were originally thought to replace teeth ideally, and even potentially to be better than teeth. Decades later, we know that is not true. Peri-implantitis, occlusal challenges, and numerous other issues have shown us that our main mission is still preservation and retention of natural teeth and that implants are a great “last resort” when teeth cannot be restored and retained (figure 4).
In-depth research needs to be accomplished on what materials would be best for dental implants and what restorative materials should be placed over implants to simulate the wear of natural teeth.
Summary
Dentistry has had several years of challenges, but many dental products and concepts needing change have stayed static. Several areas of concern are discussed in this article that need immediate attention to be overcome.
Editor's note: This article appeared in the April 2025 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.