by Mark A. Latt, DMD, MS
Modern esthetic dentistry has been catalyzed by the so-called “bonding revolution.” The ability to use tooth-colored direct and indirect resins and ceramic-based materials was fully realized as dentin and enamel adhesives were developed and their clinical performance enhanced. At their foundation, direct anterior and posterior resin composites, endodontic posts, resin cores, and laboratory processed resin and ceramic veneers, inlays, onlays, and crowns all have bonding agents that function as the bridge between the restorative material or luting cement and tooth structure.
On the surface, modern adhesive systems seem simple - merely a film to be painted on the tooth. In reality, they are often sophisticated and complicated chemical systems that have the steep challenge of interacting with the diverse molecular structures of dentin and enamel as well as with the overlying resin materials. As the key foundation for often large, tooth-colored restorations, careful attention to appropriate use and good clinical technique is essential for getting the best performance out of the bonding system and, ultimately, the restoration. Below are six key tips for getting the most out of modern bonding systems.
1) Know your bonding system
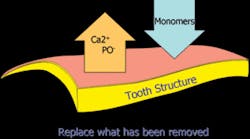
The fundamental mechanism for all modern adhesive systems is the same. Using acid or acid-resin monomers, mineral is removed from both enamel and dentin. In the spaces created by the demineralization process, resin monomers are introduced and polymerized. In both enamel and dentin, sealing, bonding, and retention is facilitated by micromechanical retention into the microporosities created during the bonding process.
Mechanism of modern bonding
In dentin, the region of the tooth where dentin is partially demineralized and resin monomers have been infiltrated around the exposed collagen is called the hybrid layer. The successful creation of this interface, especially in dentin, is critical for a long-lasting restoration without postoperative sensitivity.
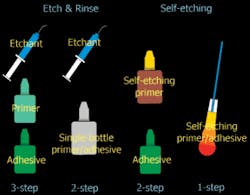
However, the large number of products and their specific differences (and often conflicting commercial claims) can make the adhesive landscape confusing for practitioners. For marketing simplicity, companies have used the term “generations” to describe new adhesive systems as they are developed and commercialized. The implication is that the higher the generation number, the more advanced - and supposedly better performing - the adhesive system will be. This, however, is not always the case. A better and more useful classification system uses the specific clinical technique to categorize the bonding system so practitioners can understand the system they use based on the materials and steps required to get the adhesive system to work as it was intended. This system is illustrated on page 54.
In this classification system, when phosphoric acid is used to condition enamel and dentin and then rinsed, these systems are termed “etch-and-rinse.” Following this, the three-step systems will place, in separate steps, a primer and adhesive from separate bottles. Examples of adhesive systems like this are Scotchbond Multipurpose (3M ESPE), OptiBond FL (Kerr), and All-Bond (BISCO).
Etch-and-rinse systems that combine the primer and adhesive into one bottle still have two steps: the acid conditioning and rinsing, and the application of the adhesive resin. Examples of bonding agents in this category include Prime & Bond NT and XP Bond (DENTSPLY), Single Bond (3M ESPE), OptiBond Solo (Kerr), Bond-1 (Pentron Clinical Technologies), and PermaQuik-1 (Ultradent).
Bonding systems categorized by their specific techniques.
Several more recently developed adhesive systems have been called “self-etching” because the adhesive system contains acid monomers that simultaneously demineralize and infiltrate the dentin and enamel. One reported advantage of these materials is the elimination of the rinsing and drying step inherent when using phosphoric acid in etch-and-rinse systems. Some of these systems use separate primer and adhesive, such as Clearfil SE Bond (J. Morita) and AdheSE (Ivoclar Vivadent), and some are one-component systems such as Prompt L-Pop (3M ESPE) and Xeno III (DENTSPLY), in which two liquids are mixed and applied to the tooth. Most recently, single-component no-mix systems have been introduced, such as Xeno IV (DENTSPLY), iBond (Heraeus Kulzer), G-Bond (GC America), and OptiBond All-in-One (Kerr).
2) Follow the product instructions carefully
Even though the fundamental mechanism for bonding is generally the same regardless of the classification of the adhesive, careful attention to the specific details of the product instructions is critical for clinical success. The critical steps needed for each system are different depending on the category of the adhesive, the number of application steps, the solvent systems, and the specific chemistry of the material to be used.
Etching time is critical with total-etch systems. When enamel and dentin are conditioned, enamel requires enough demineralization for micro-mechanical retention, and dentin should not be conditioned too long (may lead to voids under the adhesive system). For most systems, the etch time is 15 seconds. In addition, most etch-and-rinse adhesives contain solvents that must be volatilized off the tooth surface before the adhesive can be cured properly.
Self-etching systems do not require rinsing, but they may have critical steps to follow. Generally, enamel bond strength values are lower compared to etch-and-rinse systems. These systems bond better to freshly cut enamel, and bonding to uncut enamel is contraindicated for many of these materials. Some of these materials are more effective if they are applied to the surface with agitation or scrubbing. Also it is critical that self-etching systems be dried after the application step to remove the solvent and any remaining water in the adhesive film.
3) Create clinical environmental control
Creating the optimal environment for adhesive dentistry is absolutely essential for success regardless of the clinical procedure. Managing the tooth surface is even more important in bonding than in making impressions for crown and bridge restorations. Modern agents can create bonds that lead to long-lasting restorations only to surfaces free of debris, saliva, and blood.
While rubber dams are frequently used for assuring the proper isolation of a tooth to be restored, they cannot be used in some situations. The clinician should think in terms of “environmental control” before bonding, and use strategies to maintain the tooth surface so that contamination does not occur. This is especially important in the gingival box area of Class II restorations where inadequate bonding can lead to early restoration failure.
4) Don’t mix components from one system to another
Manufacturers expend tremendous effort and significant resources to receive federal approval on the safety and efficacy of dental adhesives. Mixing the primer of one system with the adhesive of another, or using a phosphoric acid conditioning step with rinsing followed by a self-etching system, are contraindicated. Dental adhesives are classified as medical devices by the Food and Drug Administration, and such mixing and matching is considered “off label” usage. This could lead to failure of the adhesive to work properly, as well as early restoration failure or even loss of the tooth.
5) Don’t mix adhesives from one manufacturer with dual-cured resins from another
There is general compatibility with all light-cured dental bonding agents and light-cured restorative materials regardless of the brand. However, when using a self-cured or dual-cured material, it is essential that the adhesive system designed for that material is used to avoid serious product failures. Self- and dual-cured resin cements, liners, and core materials contain acid-base chemistries that are sensitive to the chemistry of the adhesive systems. Acid adhesives can actually prevent the chemical-curing chemistry from allowing the cement or core material to polymerize. Some adhesive systems mix a so-called dual activator with the bonding agent to assure compatibility with the adhesive system. Some cements have specially designed self-etching adhesives that can only be reliably used with that cement system. The only sure way to prevent interference from the adhesive system when using a resin cement is to carefully follow the manufacturer’s instructions.
Care must also be exercised when using the recently introduced “self-adhesive” luting cements. While these materials are generally very good for cementing metal-supported or high-strength ceramic restorations, they exhibit significantly lower adhesion values, especially to enamel. The temptation to employ bonding systems with these systems should be resisted because while higher adhesion values may be achieved, the working properties of the cement may be altered by the interaction with the adhesive film.
6) Follow sound principles of cavity design
Because both direct and indirect bonded restorations take advantage of micromechanical retention for retention and sealing, some modifications to traditional preparation design can be made. However, careful application of fundamental cavity design parameters is still necessary for the best restoration success.
For direct composite restorations, regardless of cavity class, macromechanical retention, as originally conceived for amalgam, is not appropriate. Sharp vertical walls and line angles are not needed, and rounded internal line angles are actually preferred because it is easier to adapt resin restoratives without voids to rounded surfaces. Cavity design should be dictated by access to achieve complete removal of diseased hard tissue and access to place the adhesive system and assure proper adaptation of the restorative material to the cavity wall.
While minimally invasive cavity preparations can be used, care must be taken to gain enough visibility to determine if caries is completely removed. It is also important that all unsupported enamel be removed to prevent marginal fractures from the polymerization shrinkage inherent in the composite-curing process. Proper preparation of enamel margins, especially with self-etching adhesive systems, will maximize bond strength and improve marginal integrity.
For indirect restorations where a resin luting cement and bonding agent will be used, preparation design will be dictated more by the selection of the restorative material. Nevertheless, it is important to understand that the use of adhesive cementation does not preclude the need for proper resistance and retention form, especially for full crowns.
Conclusion
Modern dental and enamel bonding agents have allowed the promise of beautiful and long-lasting restorations to be realized. While adhesives may appear simple in their superficial appearance, creating a sound interface between the restorative material and the tooth requires careful attention to detail regardless of system type. Following sound principles of clinical technique and meticulously adhering to the specific material’s written directions are essential for successful bonding.Mark A. Latta, DMD, MS, is Associate Dean for Research and Professor of General Dentistry at Creighton University School of Dentistry. He is a graduate of the University of Pennsylvania School of Dental Medicine and the University of Maryland Baltimore College of Dental Surgery. He has been awarded numerous research grants for evaluating the laboratory and clinical performance of modern dental materials. He has lectured extensively about new dental materials and techniques, and has published more than 40 manuscripts and 150 abstracts. Reach him at (402) 280-5044, or [email protected].