Nels Ewoldsen, DDS, MSD
Discomfort during chewing and looseness are common denture complaints1 that can be addressed by liners.2-4 Denture liners with Shore A hardness ranging from 25 to 95 are classified as "soft" liners.4 Soft liners are indicated when functional and parafunctional loading produce discomfort or compromise supporting tissue health.1-3 Residual ridge morphology and bone resorption patterns affect denture support and stability. Morphological irregularities, persistent mucosal irritation, and complaints of looseness despite an intimate fit of the denture base are reasons to consider a soft denture liner.2,3, 5-7
Denture intolerance has been linked to psychological and emotional aspects of aging, loss of ability, loss of interest, and feelings of helplessness.8 Helping patients overcome denture intolerance requires treatment beyond optimizing fit and mitigating residual ridge overload. It is important for clinicians to identify and separate the functional, physiological, and psychological factors related to denture acceptance. When functional factors alone account for discomfort and tissue damage, a soft liner offers relief, minimizing ongoing damage. When denture dissatisfaction issues require differentiating functional problems from psychological factors, an interim soft liner often represents the least inexpensive, reversible measure toward a better understanding of the problems.
Interim soft denture liners are chairside formulations classified as vinyl plastisols comprised of plasticized methacrylate gels. After mixing the liquid, alcohol, and plasticizing polymer powder, the flowable but viscous mixture is placed against the denture intaglio before it begins to gel. The remarkable plasticity of these gels explains their ability to adapt to the denture-bearing areas. As gelation continues, the mixture functionally adapts well to both attached and mobile mucosa. Vinyl plastisols are effective short-term soft liners; however, the gel stiffens as plasticizer and solvent leach out, creating a crusty, porous layer within weeks. Porosity contributes to fluid absorption and staining, quickly rendering these liners unhygienic.
Room-temperature vulcanized (RTV) silicone, also used short-term as a soft liner, neither leaches chemical components nor stiffens significantly with time, but it bonds poorly to denture base acrylics and supports pathogenic biofilms.9,10 An important difference between vinyl plastisol and silicone denture liners relates to plastic and elastic behaviors after placement. Plastisols exhibit plasticity only while the plasticizer and solvent remain. Cured silicone behaves elastically, returning quickly to its original shape after being strained with very limited plasticity. Because silicone formulations contain neither plasticizer nor solvent, leaching is not a concern; however, porosity remains an issue, staining silicone liners over the course of weeks or months.
Laboratory processing improves the properties of both plastisol and silicone using temperatures and pressures exceeding what the mouth can tolerate. Laboratory processing extends clinical service life and improves adhesion of both soft liner formulations to the denture base. Disadvantages of laboratory processing include time, cost, and the requirement for stone models and molds. While neither plastisol nor silicone liners offer ideal properties, they remain the most popular chairside and laboratory processed soft liners, primarily because there are few alternatives. Systematic review of published clinical trials confirmed improved masticatory function after soft liner placement. Specifically, use of silicone liners long-term was associated with significant improvement of masticatory function parameters.7
A chemically unique, popular laboratory-processed soft liner that disappeared from the market more than a decade ago has recently returned. Polyphosphazene is a fluorinated nitrogen-phosphate elastomer distinctly different from plastisols and silicones. Novus (White Square Chemical Inc.) is a polyphosphazene elastomer unique in its energy-dispersing, elastic behavior. Polyphosphazene quickly deforms under load, converting the deformation energy into a small amount of heat before returning to its original shape. This unique hysteresis behavior likely accounts for the remarkably low incidence of postinsertion adjustments of dentures lined with Novus. Novus's unique chemistry also eliminates the biofilm adhesion problem common with silicones.4
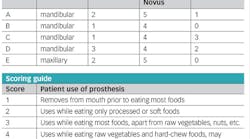
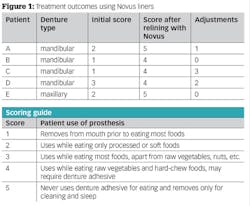
Figure 1 shows a series of five recent Novus liners completed in my private practice. In each case, the patient was asked to score the performance of their initial prosthesis. This means of assessing outcomes used a five-point scale. All of the reported patients were completed as fee-for-service treatments and all laboratory work was done at a commercial dental laboratory at published pricing.
Summary and Conclusion
While many denture wearers report satisfactory function using their prostheses, others continually report discomfort and are unable to eat even soft foods. Persistent denture discomfort is linked to poorly distributed masticatory and parafunctional loads. Residual ridge irregularities affect load distribution, concentrating stress on spiny areas and injuring the underlying mucosa. Denture soft liners cushion loads, reducing these stresses.
Thin films formed beneath denture bases by saliva or saliva in combination with denture adhesive aid denture retention. The interaction of these films with the denture surface depends on surface energy. When a denture surface exhibits low surface energy, the film adhesion potential is also low. Such is the case with silicone liners. Polyphosphazene surface energy results in better interaction with saliva and denture adhesives, resulting in superior retention, especially in patients with dry mouths.
Plastisols offer convenience of a chairside technique with short-term benefits. Tissue conditioning plastisols are an excellent first step in establishing healthy mucosa beneath the denture base. Silicone liners offer the advantage of longer clinical lives compared to plastisols. Although available only as a laboratory processed soft liner, Novus offers unsurpassed durability, consistent softness over time, and unique inorganic chemistry that makes it the best choice for denture patients with compromised salivary function and those with a history of persistent candidiasis. Novus is easily adjusted with standard rotary finishing and polishing carbides, abrasive points, and wheels. For these reasons I believe postdelivery adjustment visits and chair time are reduced significantly with high patient satisfaction.
Borders finished such that intaglio consists of Novus with cameo surface consisting of polished denture base acrylic
Comparison of conventional acrylic maxillary denture and Novus soft liner
C. albicans hyphae thrive beneath a conventional acrylic maxillary denture despite pharmacotherapy and frequent denture disinfection.
Laboratory-processed acrylic denture base supporting C. albicans
Mandibular ridge photographed at the same appointment the maxillary ridge was photographed. Note absence of C. albicans hyphae.
Novus soft liner photographed after six months at the same appointment as photo above. Note some staining is present; however, tissue health of the mandibular ridge mucosa is acceptable.
References
1. Gosavi SS, Ghanchi M, Malik SA, Sanval P. A survey of complete denture patients experiencing difficulties with their prostheses. J Contemp Dent Pract. 2013; 14(3):524-7.
2. Mack PJ. Denture soft lining materials: clinical indications. Aust Dent J. 1989; 34(5):454-8.
3. Qudah S, Harrison A, Huggett R. Soft lining materials in prosthetic dentistry: a review. Int J Prosthodont. 1990; 3(5):477-83.
4. Craig RG. Restorative Dental Materials. 9th ed. St. Louis, MO: Mosby. 1993.
5. Pereira IP, Consani RL, Mesquita MF, Nobilo MA. Photoelastic analysis of stresses transmitted by complete dentures lined with hard or soft liners. Mater Sci Eng C: Mater Biol Appl. 2015; Oct(55):181-6.
6. Hashem MI. Advances in Soft Denture Liners: An Update. J Contemp Dent Pract. 2015; 16(4):314-8.
7. Palla ES, Karaoglani E, Naka O, Anastassiadou V. Soft liners' effect on the masticatory function in patients wearing complete dentures: A systematic review. J Dent. 2015; 43(12):1403-10.
8. Golebiewska M, Sierpinska T, Namiot D, Likeman PR. Affective state and acceptance of dentures in elderly patients. Gerodontology. 1998; 15(20):87-92.
9. Anusavice KJ. Phillips Science of Dental Materials. 11th ed. St. Louis, MO: Saunders. 2003.
10. Holmer AR, Rodrigues E, van der Wielen P, et. al. Adherence of Candida albicans to silicone is promoted by the human salivary protein SPLUNC2/PSP/BPIFA2. Mol Oral Micribiol. 2014; 29(2): 90-8.
Nels EwoldseN, DDS, MSD, earned his DDS and MSD (dental materials and prosthodontics) from Indiana University School of Dentistry. He practices in Waveland, Indiana, and enjoys teaching dental students, residents, and dentists, putting his product development background to practical use. Dr. Ewoldsen has served as a consultant to dental manufacturers focusing on materials and techniques that bring better dentistry to patients, especially the underserved. A member of the Catapult Group, Dr. Ewoldsen formerly directed new technologies for GC America and clinical research for Dentsply Prosthetics.