Each month, Dr. Gordon Christensen answers a question from readers about everyday dentistry.
Q: I know implant-supported dentures are the best treatment for an edentulous person, but the cost of treatment plans is usually way above what they can afford. You have been supportive of small-diameter implants. Are they really working? I have had some surgical dentists condemn them, but I don’t know if they are familiar with the procedures.
I am placing conventional-diameter implants, but I do not have experience with small-diameter implants. Should I be using them?
A: I understand your frustration when treating low-income edentulous patients, and I also understand the dentists who have criticized small-diameter implants.
There are about 40 million edentulous patients in the US, according to the best estimates of the American College of Prosthodontists and other groups. The need for simple, relatively inexpensive procedures for edentulous patients is clear. One potential solution is now proven: small-diameter implants (SDIs) 1.8 mm to 2.9 mm in diameter.
Why were SDIs originally thought to be inadequate? Over 20 years ago, as SDIs were cleared for long-term use by the US FDA, the SDI brands available on the market were not well known. Some of them were pure titanium, which was not strong and bent easily in service. Some orthodontists were using SDIs as temporary anchorage devices (TADs) for orthodontic tooth movement. They were designed to be taken out when the anchorage was not needed.
There was significant confusion about using SDIs as final support for removable dentures. Having placed conventional-diameter implants (3 mm or greater in diameter) for many years at the time the SDIs started to come on the market, I was having the same frustration you expressed in your question. I started using SDIs frequently for situations where there was minimal bone, or when the patient did not have adequate financial ability. Eventually, I expanded my use of SDIs to the following types of patients, most of whom did not have adequate funds for complex treatment:
- Inadequate bone quantity and no patient interest in major grafting
- Inadequate bone quantity and lack of patient financial ability for major grafting
- Inadequate bone quantity and patient too physically debilitated for major grafting
- Adequate bone quantity but patient too physically debilitated for conventional implant placement
- Patient wants minimally invasive procedure without removal of crestal bone, usually required for some “all on X” techniques
A few years passed, and I was seeing almost no failure of SDIs. I published papers on the topic about my observations, which were still under criticism mostly by those dentists who had not accomplished the procedures. Controlled comparative studies started to be published showing survival of SDIs equal to or even better than that of conventional-diameter implants.
Note: This editorial is not intended to be a scientific article, but if you are interested you can go to PubMed yourself to find the research.
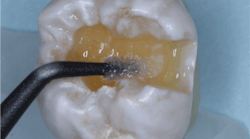
The more recent advent of peri-mucositis and peri-implantitis around implants showed some important and surprising results. The one-piece SDIs placed along with conventional-diameter implants in the same mouths at the same time by the same clinician did not show the same periodontal disease around the SDIs (figure 1). This finding stimulated my interest in SDIs not only for low-income patients, but also as a viable alternative for any edentulous patient.
Clinical suggestions for clinicians interested in using SDIs
- Bruxers or clenchers are not good implant candidates.
- Bone quantity. 4 mm of bone facial-lingual and 13 mm of bone crestal-apical are minimal desirable characteristics.
- Bone quality. 30 Ncm or more of resistance on insertion is a minimal desirable characteristic.
- Width of implant. Leave 1 mm of bone facial and 1 mm lingual.
- Length of implant. 13 mm is desirable. Shorter SDIs are questionable.
- Soft tissue coronal to the bone. Prefer only 2 mm of soft-tissue coronal to the bone.
- More than 15 degrees of nonparallelism can create undesirable implant movement on denture insertion.
- Separation of implants. Leave space for the housings, abutments, or attachments; usually 4 mm of space between implants is minimal.
- Immediate loading of SDIs is most common. If questionable bone, let implants integrate before loading. Line with soft denture liner.
Primary locations in the mouth for SDI use
The following data is from a questionnaire study published by Clinicians Report (CR).1 CR survey results (n=805) for SDIs are listed in order of most to least use. Percentages equal more than 100% since multiple answers were possible.
Current advice from CR consultants and CR staff is that items 1–6 below are proven uses for SDIs, while techniques 7–9 need more long-term research and development.
- Edentulous mandible removable complete denture (figure 2): 86%
- Edentulous maxilla removable complete denture: 34%
- Partially edentulous mandibular removable partial denture: 30%
- Single mandibular incisor replacement: 26%
- Single maxillary lateral incisor replacement: 21%
- Partially edentulous maxilla removable partial denture: 19%
- Replacement of missing single posterior teeth with implant-supported crowns
- Fixed partial dentures
- Fixed or fixed-removable prostheses for edentulous patients
Popular example brands (figures 3 and 4)
- Dentatus
- Glidewell Laboratories
- Intra-Lock (MDL)
- Noris Medical
- Shatkin F.I.R.S.T
- Sterngold (MOR)
- Straumann
- Zest Anchors
Typical technique for edentulous mandible
- Diagnostic appointment. Cone beam is now considered to be standard of care for implant placement.
- Patient informed consent
- Alternative treatments for care
- Advantages of each
- Disadvantages of each
- Risks of each
- Costs of each
- What happens if you do nothing?
- Place four implants in anterior mandible (figure 5). Per CR survey data, about 80% are placed without a flap.
- If a flap is done, wait several weeks before impression to allow soft-tissue healing. During that time, use soft reline material in the patient’s old denture in areas where the implants were placed.
- Make a conventional denture and pick up implant housings in the denture at seating or rebase of previous old denture, if it is acceptable.
- If a flap is not done, load immediately if desired (figure 6).
- Adjust the denture as needed, about twice, one week apart.
Summary
One-piece small-diameter implants (minis, SDIs) have been proven to work as well as or better than conventional-diameter implants for some clinical situations. They are minimally invasive, simple to place and restore, and relatively inexpensive especially for implant-supported and retained mandibular complete dentures.
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic.
One-hour videos:
- Proven Simple and Successful Use of Mini Implants (Item #V2305)
- Simple, Inexpensive Implant Solutions for Edentulous Mandibles (Item #V2388)
Two-day hands-on courses in Utah:
- Faster, Easier, Higher Quality Dentistry with Dr. Gordon Christensen
- Implant Surgery – Level 2 with Dr. Gordon Christensen
- Simplifying Complex Treatment with Dr. Gordon Christensen
For more information, visit Practical Clinical Courses or call (800) 223-6569.
Editor's note: This article appeared in the March 2024 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
Reference
- When and where should small diameter implants be used? Clinicians Report. 2016;9(6).
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, RDH, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.