After many years of general dental practice, I see some of my crowns lasting for decades and others failing after a few years. You have many years of experience. What are your conclusions on the factors that affect crown longevity?
Practicing any health profession is named appropriately; we don’t know exactly why some procedures are successful or not without years of observational research. We must share our experiences, accumulate those observations in an organized manner, and make conclusions. Such in vivo research is then published, and, at least for a short period of time, that research is valid, until materials, technologies, and techniques change. Long-term evidence is essential.
Read more about crowns ... Successful cementing of zirconia crowns: Still a problem
After practicing for several decades and observing thousands of crowns serve and eventually fail, I have come to some conclusions that I’ll share with you here. These are based on personal experience as well as research from the dental literature and Clinicians Report Foundation. This information will provide guidance relative to treatment planning and treatment for crowns.
Diet
The diet of some people is conducive to caries. This should be evident when observing a mature patient with existing restorations. Some people have lived to maturity without any caries or periodontal disease, while others have had large direct restorations or crowns and ongoing periodontal disease. Can diet be changed? Yes, but only with continuing patient education and only for some people. Cariogenic diets contain high sugar both in fruit and in processed sugar that’s added to almost everything we eat. Will that change? No, but it can be reduced by educating motivated patients. Sticky, sugar-containing foods have been shown to be the worst for promoting caries, because they stay on the teeth longer than liquids. Educate your patients!
Oral hygiene
Patients with many previous restorations have almost always had high-sugar diets and inadequate oral hygiene. Can this challenge be reduced? Yes, but usually only for the short term even when combined with constant oral hygiene instruction. If you observe many restorations on a new patient, your immediate treatment planning should consider subgingival margins for crowns, cariostatic cements, 5,000 ppm toothpaste, and potentially more frequent recare appointments. Assuming the patient can improve their oral hygiene and you’ve used optimum cariostatic materials and oral hygiene procedures, crown longevity will be increased.
Tooth preparation
If you were to visit a large dental laboratory and observe tooth preparations, you would be convinced some crown preps could be significantly better. Why are some preps inadequate? Dental schools have too much to teach, and some dental students have minimal clinical experience and treatment speed at graduation. The combination of minimal clinical experience, the pressure to produce enough revenue to pay the bills, and reluctance to attend continuing education courses are some reasons for inadequate crown preparations.
What is an acceptable crown preparation? The following information includes tooth preparations for the two most frequent types of crown materials: zirconia and lithium disilicate.
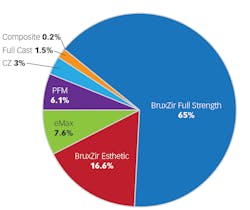
Zirconia: Most crowns placed today are zirconia (figure 1) of various formulations (personal communication, Darryl Withrow, Glidewell Laboratories). Zirconia has high strength but also numerous formulations influencing and reducing strength.1
Currently, the most frequent procedures are crown preparations made with low-cost diamonds2 (DollarDiamonds, NeoDiamond, Solo, etc.), impressions made with polyvinyl silicone3 (Aquasil Ultra, Imprint 4, etc.) that are subsequently scanned by laboratories, and crowns cemented with resin-modified glass ionomer cement4 (RelyX Luting, FujiCem Evolve, etc.).
Figures 2–4 show crown preps for zirconia and lithium disilicate as reported in numerous articles in the literature and in Clinicians Report.
Zirconia prep characteristics:
- Axial walls no more tapered than 20 degrees from the tooth long axis
- Axial walls 0.6 mm to 1.0 mm deep
- Slight chamfer margins
- Occlusal reduction of 1.5 mm to 2.0 mm
- Primary anatomy on the occlusal table
Lithium disilicate: This material is weaker than zirconia of any current variety, so the prep must be deeper for the strength of the restorative material (figures 3 and 4).
Lithium disilicate prep characteristics:
- Axial walls no more tapered than 20 degrees from the tooth long axis
- Axial walls 1.0 mm deep
- Moderate chamfer margins
- Occlusal reduction of 2.0 mm
- Primary anatomy on the occlusal table
Location of crown margins
If the patient has had minimal caries, some crown prep margins can be supragingival and left on enamel. If the patient has had lots of caries previously, I suggest the margins should be about one-half of the way into the gingival sulcus. Subsequent caries usually occurs quickly on dentinal supragingival margins in caries-active patients.
Crown material
Locations for full-strength, LT, 3Y, tetragonal, and class 5 zirconia
These names are now in circulation for the strongest type of zirconia, but they’re confusing. Based on current research from the TRAC division (Technologies in Restoratives and Caries Research) of Clinicians Report Foundation, this type of zirconia is preferred on molars. Currently, however, companies are promoting the slightly more esthetic but weaker 4+Y types described in the next section.1
The main locations for use of this material:
- Fixed prostheses, especially long-span fixed prostheses
- Bruxing patients, preferably all teeth using color-modified class 5 in the anterior segment
- Any location where heavy occlusal forces are anticipated
Read more about crowns ... How to reduce recurrent caries and crowns coming off
Potential locations for 4, 5 and 5+Y, HT, esthetic, cubic, and class 4 zirconia
These names are now in circulation for the slightly more esthetic, but weaker zirconia formulations. Current TRAC research about these materials is mixed. Some are excellent, and some are breaking after a few years.
Some tips:
- Provide patient education and get patient informed consent.
- The locations most indicated are those in the patient’s smile zone.
- Use for premolars, especially maxillary, but some mandibular.
- Use for anterior teeth, maxillary and mandibular.
- More research is needed to validate fixed prostheses.
- More research is needed for bruxing patients.
Locations for lithium disilicate (IPS e.max)
Lithium disilicate restorations now have more than 12 years of international use and excellent research showing over 95% clinical success for single crowns based on TRAC research.
The main locations for use of this material:
- Single teeth in nonbruxing patients, anterior and posterior if thick enough (1 mm axial and 2 mm occlusal)
- Selected three-unit fixed prostheses, premolar and anterior
- Veneers
- Avoid placing in bruxing patients.
Cement
Resin-modified glass ionomer (RMGI) has been shown by Clinicians Report Foundation scientists to have fewer zirconia crowns come off in service than resin cement, despite the higher strength of resin cement.5 The rigidity of RMGI is probably the reason.
Resin cement is usually preferred for lithium disilicate because of its higher strength than RMGI, color variability, and ease of use. However, in caries-active patients, if all aspects of the crown prep are 1 mm or more deep, RMGI can be used in nonbruxing patients.
Contact areas and overall crown anatomy
Broad, flat, tight contact areas reduce the possibility of food collecting interproximally. I often see contact areas slightly loose with food packed in the interproximal areas and resultant caries and periodontal disease. Specify tight contacts to the laboratories you use. It’s easy to slightly loosen the contact if it’s too tight.
Occlusion
Both zirconia and lithium disilicate are unforgiving if occlusion is too high, causing potential damage to opposing teeth and occlusal dysfunction. Make sure you adjust any high spots carefully!
Summary
Based on my observations of thousands of crowns over several decades of practice, as well as information from scientific studies, crowns can have long-term esthetics, optimum function, and patient satisfaction if you utilize the information in this article.
Editor's note: This article appeared in the September 2023 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
Author’s note: These educational materials from Practical Clinical Courses offer further resources on this topic.
One-hour videos:
- Strong, Comfortable, Esthetic Rehabilitations with Zirconia (Item #V1942)
- Cementing Restorations—Proven & Successful (Item #V1921)
Three-hour virtual course:
- Removable Prosthodontics—Predictable & Enjoyable (Item #X2553)
Two-day hands-on courses in Utah:
- Simplifying Complex Treatment with Dr. Gordon Christensen
- Restorative, Esthetic, Preventive Dentistry with Dr. Gordon Christensen
For more information, visit Practical Clinical Courses website or call (800) 223-6569.
References
- Christensen GJ. New crown classification system arises from zirconia changes. Clinicians Report. 2019;12(7).
- Christensen GJ. Clinical performance of low-cost diamonds. Clinicians Report. 2018;11(8).
- Christensen GJ. Impressions made with polyvinyl silicone. Clinicians Report. 2023;16(8).
- Christensen GJ. Cements 2022: concrete suggestions for every restoration. Clinicians Report. 2022;15(4).
- Christensen GJ. Rescue techniques for failing restorative treatment. Clinicians Report. 2018;11(7).