Metabolic syndrome and its impact on periodontal disease and dental implant disease
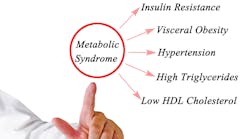
Metabolic syndrome (syndrome X, insulin resistance) is a multifactorial disease with multiple risk factors arising from insulin resistance leading to abnormal fat tissue deposition and function. Consisting of several conditions and diseases that occur together, metabolic syndrome increases the risk for cardiovascular disease and more than doubles the risk of developing type 2 diabetes. Until recently, little was published regarding the association between metabolic syndrome and oral disease, such as periodontal disease and peri-implant disease. This article will briefly describe the definition of metabolic syndrome, risk factors and conditions, and the impact this disease has on periodontal disease and dental implant disease.
Also by the author:
- Reducing the need for adjunctive antibiotics during scaling and root planing
- Pinhole Surgical Technique: A 10-year evaluation of root coverage
What is metabolic syndrome?
By definition, metabolic syndrome is a cluster of conditions that requires the individual to have at least three of the following risk factors at the same time:
- Increased abdominal circumference
- Low plasma levels of high-density lipoprotein cholesterol
- Increased values for plasma triglycerides
- Elevated blood pressure
- Elevated glucose levels.1
More specifically (three out of five conditions needed):2
The prevalence of this disease has shown an increased trajectory over the years similar to diabetes and is estimated to affect more than 25% of the adult US population.3 More recent publications estimate this disease to affect approximately 34% of the adult US population and 10% of the adolescent US population.4 That would mean that an average of one out of every three patients treated in a dental office could be affected with metabolic syndrome.
What are the risk factors for metabolic syndrome?
Metabolic syndrome is thought to be caused by adipose tissue dysfunction and insulin resistance, and therefore, the predominant underlying risk factors for metabolic syndrome appear to be abdominal obesity and insulin resistance.5 Most inflammatory diseases—including periodontal disease6 and diabetes—that heighten inflammation, increase cytokine production, lead to oxidative stress, and lead to glucose/lipid toxicity and resistance have been associated with metabolic syndrome.7 Other associated conditions are diet, genetics, physical inactivity, aging, and hormonal imbalance.2
Metabolic syndrome and periodontal disease
Periodontal disease is a chronic inflammatory disease associated with dysbiotic plaque biofilms and characterized by a progressive destruction of the proximal tooth-supporting apparatus.8 Because both periodontal disease and metabolic syndrome have been associated with elevated inflammatory markers such as C-reactive protein and IL-6, research has suggested that periodontal disease can exacerbate the severity of metabolic syndrome.9 Similarly, it has been hypothesized that periodontal therapy may decrease the inflammatory state of the patient, which can aggravate metabolic syndrome and thereby improve therapeutic outcomes when trying to control metabolic syndrome.10
In addition, it has been concluded that metabolic syndrome and periodontal disease can influence one another due to the reciprocity between dysbiosis of the oral and gut microbiomes.11 Metabolic syndrome can alter the oral microbiome, leading to a dysbiosis that can exacerbate the severity of periodontal disease. Gut dysbiosis and alteration of the gut microbiome has been associated with heightened metabolic syndrome. Periodontal disease and oral dysbiosis can lead to gut dysbiosis, thereby influencing the severity of metabolic syndrome.
Metabolic syndrome and peri-implant disease
Because metabolic syndrome is associated with both a proinflammatory state and a dysbiosis of the gut and oral microbiome, bone metabolism can be affected by this disease. Notably, an increase in osteoclastic activity and a decrease in osteoblastic maturation is seen. This disruption of bone homeostasis favoring bone resorption is thought to be the result of a dysfunction in insulin receptor seen in individuals with metabolic syndrome, as insulin resistance can cause hyperinflammatory states.12 Hyperglycemia is also often seen with metabolic syndrome leading to a potential vascular impairment and delays in angiogenesis and wound healing. Poor wound healing and bone metabolism favoring bone resorption can lead to peri-implant disease and attachment loss around a dental implant, especially when there is a bacterial challenge present.13
One study evaluated 183 patients with implants and found that peri-implant bone loss occurred in 37% of patients with metabolic syndrome compared to 25% of patients without metabolic syndrome. The authors concluded that patients with metabolic syndrome are more likely to experience bone and gum problems around their dental implants, but more studies are needed. In general, because metabolic syndrome is a disease that is increasing at a high rate, more research is needed to evaluate the relationship between periodontal and peri-implant disease and metabolic syndrome.
Editor's note: This article appeared in the September 2022 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Stone NJ, Bilek S, Rosenbaum S. Recent national cholesterol education program adult treatment panel III update: adjustments and options. Am J Cardiol. 2005;96(4A):53E-59E. doi:10.1016/j.amjcard.2005.06.006
- Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112(17):2735-2752. doi:10.1161/CIRCULATIONAHA.105.169404
- Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol. 2008;28(4):629-636. doi:10.1161/ATVBAHA.107.151092
- Moore JX, Chaudhary N, Akinyemiju T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Prev Chronic Dis. 2017;14:E24. doi:10.5888/pcd14.160287
- Goossens GH. The role of adipose tissue dysfunction in the pathogenesis of obesity-related insulin resistance. Physiol Behav. 2008;94(2):206-218. doi:10.1016/j.physbeh.2007.10.010
- Srivastava MC, Srivastava R, Verma PK, Gautam A. Metabolic syndrome and periodontal disease: an overview for physicians. J Family Med Prim Care. 2019;8(11):3492-3495. doi:10.4103/jfmpc.jfmpc_866_19
- Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;(219):1-8.
- Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S173-S182. doi:10.1002/JPER.17-0721
- López NJ, Quintero A, Casanova PA, et al. Effects of periodontal therapy on systemic markers of inflammation in patients with metabolic syndrome: a controlled clinical trial. J Periodontol. 2012;83(3):267-278. doi:10.1902/jop.2011.10.110227
- Gobin R, Tian D, Liu Q, Wang J. Periodontal diseases and the risk of metabolic syndrome: an updated systematic review and meta-analysis. Front Endocrinol (Lausanne). 2020;11:336. doi:10.3389/fendo.2020.00336
- Pirih FQ, Monajemzadeh S, Singh N, et al. Association between metabolic syndrome and periodontitis: the role of lipids, inflammatory cytokines, altered host response, and the microbiome. Periodontol 2000. 2021;87(1):50-75. doi:10.1111/prd.12379
- de Oliveira PGFP, Bonfante EA, Bergamo ETP, et al. Obesity/metabolic syndrome and diabetes mellitus on peri-implantitis. Trends Endocrinol Metab. 2020;31(8):596-610. doi:10.1016/j.tem.2020.05.005
- Froum SJ, Rosen PS, Wang WC, Froum SH, Vinayak S. Retrospective evaluation of factors related to the outcomes of regenerative therapy for implants affected by peri-implantitis. Int J Periodontics Restorative Dent. 2018;38(2):181-187.doi:10.11607/prd.3489