Managing periodontics into a successful practice of dentistry
by Samuel B. Low, DDS, MS, MEd
While many practices effectively incorporate periodontal therapy into the comprehensive management of their patients, some practitioners deal with the frustration of return on investment. This may be due to lack of appropriate training, including team members, in managing periodontal patients on a day-to-day basis, patients who cannot appreciate periodontal disease and the subsequent treatment due to being asymptomatic, or not having an understanding of the potential growth niche of periodontics in the overall practice structure.
One of Dr. Pankey’s favorite phrases was, “Do what you do best, and the money will come.” This article will provide the practitioner with a primer of practice management skills to provide not only quality periodontal therapy, but also the financial rewards as the positive side effect.
Periodontal disease is not just about bugs
Many of us grew up in our dental education experience appreciating that the primary etiology of periodontal disease was microbial in nature. Drilled into our dental student heads was “no plaque, no disease.” Recent evidence justifies that the bacterial etiology is only a stimulus to initiate an inflammatory reaction. This response results in the host’s defense cells releasing mediators that disrupt the function of healthy connective tissue. Therefore, there is more similarity in the nature of subgingival biofilms from patient to patient than the host reaction from patient to patient. With periodontitis being a chronic inflammatory disease, the word treatment should be removed from the dental vocabulary and replaced with management.
Understanding periodontitis as one of several chronic inflammatory diseases changes the landscape on management. Three critical concepts in managing both the host and the microbial etiology become evident:
- Subgingival biofilms are a mainstay in the progression of periodontitis. They are highly complex in nature with an ecosystem evolved for survival. Their disruption requires not only mechanical removal, but also a follow-up that is medicinal in nature.
- Site-specific pocket depths are the nature of the geography of periodontitis. On average, a periodontitis patient has 15% of the sites that are inflamed, with a natural predilection for the molar teeth.
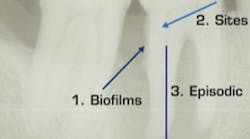
- Episodic progression of moderate to severe disease can be related to the systemic nature of the host (Fig. 1).
Perio pearl: Balance antimicrobial with anti-inflammatory in managing your periodontal patients.
Fig. 1 — Major periodontal concepts
Five commitments for periodontal practice management
I. Commit to a comprehensive periodontal evaluation
A quality periodontal evaluation includes periodontal probing with furcation assessment (Fig. 2), a radiographic exam that must include posterior vertical bitewings, tissue characteristics such as the level of attached gingivae, and mobility patterns. These areas are further defined in the recent American Academy of Periodontology 2011 Statement on Comprehensive Periodontal Therapy at www.Perio.org. The effective practitioner explains to the patient in detail the reason for periodontal charting, what the numbers imply, and management systems for the respective diagnosis. Unmanaged periodontitis should be described as resulting in not only tooth loss, but also “erosion of the jawbone.” Again, there are few if any symptoms of progressive periodontitis, and the practitioner must educate if the patient is to accept short- and long-term management.
Fig. 2 — Periodontal charting with radiographs
If the host is truly part of the equation in progression, the clinician will consider the following questions as a “checklist” in evaluating the host:
- Who was your previous dentist, and how was the experience?
- Were there any symptoms of gum disease?
- Has any dentist ever mentioned gum disease to you?
- When was your last “cleaning”? How frequently did you undergo these “cleanings”?
- Do your brothers, sisters, or parents have any history of gum disease?
- Do you use tobacco?
- Do you grind or clench your teeth?
Studies demonstrate that approximately one-third of the adult population is predisposed to periodontitis. If the average dental practice has approximately 1,800 patients, then 600 patients possibly have periodontitis. The clinician’s objective is to determine which patients have periodontitis, which teeth have periodontitis, and which sites have periodontitis, and then document it in graphic charting systems to assist in management. We recommend color-coding charts with stickers, with green stickers for gingivitis patients (possibly the 1,200) and red stickers for the periodontitis patients (600). The color coding signifies to all of the team members in the practice the diagnosis and therefore the corresponding management.
A periodontal charting system should be legible and user-friendly to the degree that it could be distributed to the patient along with digital copies of their radiographs for their records. Color coding site specific disease on images of teeth shows all stakeholders the sites and degree of the progression of pocket depth and furcation involvement. Several data entry systems are available through Florida Probe to assist the clinician in effectively collecting periodontal pocket depths, etc. These systems become the roadmap for not only demonstrating the patient’s disease state, but also leading into case acceptance by visual, nonverbal objective cues (Fig. 3).
Fig. 3 — Florida Probe Periodontal Exam Chart
Perio pearl: Maximize perio data collection by having charting systems and radiographs very patient-user-friendly so that the info sells case acceptance.
II. Delegate effectively to the dental hygienist
The dentist determines the level of periodontal disease for the patient and the subsequent management system. However, the dental hygienist as part of the team provides input into the management plan, as well as implementation of the plan at chairside. There are many facets to a periodontal treatment plan, with the most significant being biofilm control both from oral hygiene and chairside, and management of the host with consideration of genetics, nicotine, diabetes, occlusion, and overall systemic conditions.
The cornerstone of a successful practice is relationship building with patients. It is a mandate that the dental hygienist review the patient’s chart in detail prior to seating the patient so that he or she is familiar with the patient’s status. One suggestion is that the practice offer patient orientation at the beginning of each practice day. This increases efficiency, and patients appreciate knowing that the hygienist is familiar with their conditions prior to treatment. Dentists performing treatment plans in dental hygiene operatories should be held to a minimum since this is the No. 1 contributor to why dental hygienists do not stay on schedule. When dental hygienists perform periodontal charting, a second staff member entering periodontal data is essential from a time and accuracy perspective.
If we consider the concept that one-third of our patients have periodontitis, then the debridement procedure must be related to the management system for that diagnosis. At a minimum, one-third of the patient base of an average practice should be considered to receive periodontal debridement, i.e., scaling and root planing. Two-thirds of the patients may receive a gingival debridement, i.e., prophylaxis. A simple analysis of a practice management software system can determine the percent of patients receiving appropriate management.
On occasion, an audit will reveal that a practice is under 15% in managing periodontitis, according to third-party coding. This can be the result of performing prophylaxis on periodontitis patients, and/or performing periodontal debridement on periodontitis patients and charging prophylaxis fees. Unfortunately, the latter happens frequently due to the practice being afraid that the patient may not return and the practice will therefore lose revenue. By changing the practice culture of educating patients about their periodontitis and its ramifications, root planing fees can be assessed with the resulting increase in return on investment.
Perio pearl: Establish the necessity/value of a perio debridement over a “prophy cleaning” by describing consequences as not only tooth loss and systemic effects, but “the erosion of the patient’s jawbone.”
III. Commit to the phase I evaluation
The nature of management requires observation versus direct treatment, which generally has a definedThe objective of phase 1 therapy is to reduce the inflammatory nature of periodontitis to the level that it can be managed nonsurgically with frequent maintenance recare. Valid and reliable metrics with pocket depth are the primary measurement of periodontal health. Pre- and post-changes provide the clinician with a benchmark of future management. A time frame for consideration is approximately six to eight weeks following the scaling and root planing (debridement) procedures. At the phase 1 evaluation, the clinician reprobes all sites and determines if there has been a positive, negative, or no change in measurements. Decrease in pocket depth to 4 mm or less in areas of single rooted teeth with horizontal bone loss can generally be maintained. Final phase 1 evaluation pocket depths greater than 4 mm in posterior areas with angular osseous topography will require additional intervention such as surgical modalities. Therefore, a decision tree can be developed at the phase 1 evaluation that includes three possible options: 1) maintenance, 2) surgical intervention, or 3) recycle through phase 1 again due to oral hygiene compliance. Documentation is essential for patient management and risk management.
Perio pearl: Utilize perio checklists and flowcharts posted and readily available in all areas so that the team is well aware of management protocols and the future direction for the patient.
IV. Commit to the recare appointment
To maximize quality patient care with the resulting increase in financial gain, the practice must move beyond the culture of routine cleanings. Eliminating the word “cleaning” from the practice vocabulary is the first step in maximizing the potential of the recare appointment. Consultants such as Roger Levin have maintained that 50% of case acceptance for major restorative dentistry occurs in the dental hygiene recare operatory. As suggested earlier, it is critical that the dental hygienist be aware of the suggested treatment plan, be knowledgeable of the procedures, and be able to reinforce the treatment plan. Subtle engagement with the patient can trigger a dialogue and subsequent acceptance of procedures.
Smart practices help team members with leadership characteristics, including the ability to communicate and develop positive relationships. The dental hygienist is a critical team member because he or she has significant quality time with patients on a frequent basis. We consider the 60-minute recare appointment as a pie chart, with allocation of minutes based on priorities of therapy. Attempting to decrease the time of the recare appointment creates ineffective time management, with no opportunity to engage the patient in a discussion of their care (Fig. 5).
Again, legible documentation is critical to provide quick reference about a patient’s history in the practice. One suggestion is to provide a boilerplate format in which the dental hygienist and dentist insert their notes. The use of graphics, including color coding, adds to the time effectiveness and accuracy in the management (Fig. 6). Patients should leave the practice appointment feeling they had a meaningful interaction and assessment of not only their oral health, but also their systemic health by reviewing their medical history, including medications and such metrics as blood pressure and pulse.
Maintenance intervals should be based on diagnosis, risk assessment related to host susceptibility, and oral hygiene compliance. The cookie-cutter three-month recare is outmoded and should be replaced with a customized system based on individual patient status.
Perio pearl: At recare, the hygienist becomes the patient manager and must be fully aware of all past and present medical/dental history of the patient, including areas of concern prior to the dentist’s entering the recare operatory.
V. Commit to a dialogue with a periodontist
The patient is always under the management of the general practitioner. Referral is based on a decision by the dentist. If there is persistent periodontal inflammation following phase 1 therapy, especially with pocket depths of 5 mm or greater, a consideration for surgical intervention should be part of the decision tree regardless of who renders the therapy.
Open communication between the referring dentist and the periodontist is critical for effective management. Dentists who provide the periodontist with diagnostic quality radiographs and data that includes the dentist’s concerns of the oral conditions, potential restorative treatment plan, medical complications, and compliance prepare the periodontist with the information to enhance the mutual management of the patient.
Developing a relationship with a periodontist takes time and should be built on trust and communication. Similar philosophies of management with practice styles that enhance quality patient rapport are a given in building these relationships.
Periodontal patient management can be an extremely rewarding component of a vibrant dental practice. The practice management process that coincides with the periodontal aspects is what brings the rewards to fruition.
Dr. Samuel Low is professor emeritus, University of Florida, and associate faculty of the Pankey Institute with 30 years of practice in periodontics and implants. He is past president of the American Academy of Periodontology and Florida Dental Association (FDA), “Dentist of the Year” by the FDA, and distinguished alumnus of the University of Texas. He received the Gordon Christensen Lecturer Recognition Award and is presently 17th District ADA trustee. Contact him at [email protected].
Past DE Issues