Quality of care has long been considered paramount in the profession of dentistry. Starting in dental school, each dentist, in some way or form, personally assesses the quality of his or her work. How well a restoration is contoured, the bevel quality of a crown preparation, the speed with which each appointment is completed-these are just a few of the thousands of ways dentists think through quality of care. But while these individual assessments serve as one means of evaluation, they ultimately prove subjective in nature and do not necessarily lead to productive practice translation.
Quality assurance
Health-care professionals desire to meet a standard of care that is defined by laws, regulations, professional ethics, and ideals. A good quality assurance policy or protocol provides the most direct means to assess standard of care while allowing for the discovery of nuances in professional practice.
A quality assurance plan must include the progression of quality assessment, identification of issues, development of a strategy for resolving problems, and implementation of changes.1-2 At the end of each quality evaluation period, providers and staff should have information to develop new policy and practice modifications that will lead to positive performance improvement.
Measuring performance improvement
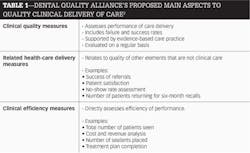
As seen in Table 1, the Dental Quality Alliance (DQA) proposes three main categories for assessing quality in clinical delivery: (1) clinical quality, (2) related health-care delivery, and (3) clinical efficiency.3 These three categories allow for both a quantitative and qualitative assessment that should lead to performance awareness and improvement.
Assessment of current quality systems being used in dentistry reveals a strong tendency toward quantitative evaluation. This is true for multiple reasons. For example, the professional system leans heavily toward efficiency. Moreover, clinical output has become a measure of success.
It is a much easier process to measure efficiency and output rather than effectiveness due to few evidence-based guidelines, limited outcome knowledge, and data accessibility issues.3-4 However, when clinical output is singularly used to determine success, desired outcomes and goals can be skewed or even missed.
READ MORE | How to effectively incorporate intraoral cameras into your practice
Developing a Performance Improvement-Quality Assurance Plan
When developing a Performance Improvement-Quality Assurance plan (PI-QA), it is advantageous to draft a basic mission and vision statement. This statement should reflect ideals and goals while defining what the practice/program is all about.
Statements can be as simple as the following: "Our mission is to provide the highest quality care while maintaining financial sustainability. Our vision is to continue this into the future." Alternatively, statements can be more complex and specific to the practice's identity. The point is to have a foundation that ties into the practice's identity and allows for quality assurance measures to be copacetic with the practice's vision.
The next steps are to set up methods for identifying and evaluating quantitative and qualitative aspects to care.
Quantitative measures
Quantitative measures are seen most often in dentistry and usually focus on the profit/loss report. While monthly profit/loss reports are vital to operations, revenue and/or cost-per-encounter data can provide more detailed information.
Revenue per encounter
Revenue per encounter can be used to assess more specific efficiencies using simple cross-referencing with parameters such as the following:
- Changes in cost with patient type (e.g., age, systemic illness, obesity)
- Differences in revenue with auxiliaries and front office personnel (e.g., cost using one assistant versus another, intra-office communication between personnel)
- Differences in type of care appointment (e.g., restorative versus emergency care)
Additional quantitative measures
In addition to profit and loss, other common quantitative measures include:
- Number of patients seen
- Number of procedures used
- Number of relative value units (RVUs)
RVUs are most typically associated with corporate, group, and organizational-based dental care delivery. RVUs assign a numerical value to each dental procedure as a means for production and cost analysis.5-6 The goal of RVUs in dentistry is to provide a standardized unit of effort for differing procedures of care.6 More information on RVUs can be found at www.dentalclinicmanual.com/chapt5/3_9.html.
EU3
(CDT code D0145)
Oral evaluation for patient under the age of 3 yearsLOE
(CDT code D0140)
Limited oral evaluation (problem-focused examination)POE
(CDT code D0120)
Periodic oral evaluationCOE
(CDT code D0150)
Comprehensive oral evaluation
Treatment plan completion
Treatment plan completion (TPC) relates to the elimination of disease that allows the patient a more effective pathway for disease stabilization and prevention.5 TPC is calculated by evaluating total numbers of completed treatment reports with evaluations performed (EU3, LOE, POE, COE) or the total number of patients seen within a set time period. This is usually tracked by creating a "dummy code" in a site's electronic dental record that can be accessed via electronic reporting.
For example, take the case of a new patient entering the practice and receiving a comprehensive evaluation. The patient needs one restoration, the standard prophylaxis, radiographs, etc. Once the patient has completed all care, a dummy code (such as TXCOMP) is entered into the patient's chart. (Note: If a patient only requires preventive care, then once preventive care is finished, the treatment plan should be considered complete and the dummy code inserted into the patient's chart.)
Most electronic dental software programs offer a means to report on these dummy codes. They can even be sorted by billing type or type of procedure code performed (figure 1). Nationally accepted benchmarks for TPC rates do not exist. However, highly effective dental programs have demonstrated a range of 60% to 75% completion rate in a 12-month period.5
Dental referral process
In comparison to the health-care system as a whole, evaluation of the dental referral process demonstrates that the profession is lacking in both quality of referral and consistent tracking of completed referrals.7
The ability of health-care providers to directly assist in completing referrals is linked to positive patient outcomes and increased patient satisfaction.8 The advantages to tracking met referrals for the dental provider are:
- Provides information on the referred providers (e.g., cost, patient perception, treatment process)
- Can depict the needs of a patient base (i.e., if only a small percentage of patients are able to complete orthodontic referrals, then a solution may be to focus on acquiring these skills through additional training)
- Uncovering the overall needs of the community (e.g., patients referred for hypertension are not able to be seen locally, operating room time cannot be secured for pediatric patients)
By understanding the environmental challenges to care access, a practice can determine where needs exist and attempt to fill those needs.
Qualitative measures
The dental profession is in the very early stages of incorporating quality evaluations. Previous proposals have focused on providers using peer review to establish when standard of care is met,5,9 periodic chart reviews/audits,10 and patient satisfaction reviews/surveys,11-12 all of which have moved the needle forward but not reached universality.
One proposed method that is gaining widespread traction relates to caries risk assessments.13 The American Dental Association (ADA) recently added caries risk coding to the CDT nomenclature (D0601 for low caries risk, D0602 for moderate caries risk, and D0603 for high risk). Risk-based care focuses on the patient's current oral health description to facilitate specific care and intervention.
Currently, three caries risk determinant tools have garnered the most use: Caries management by risk assessment (CAMBRA), the ADA age-based risk assessment, and the American Academy of Pediatric Dentistry risk assessment tool.14 Their use varies depending on provider preference, and true validity of these tools does not currently exist. However, their use as a quality measure can hold value-especially if used in a consistent manner within a single practice.15
One way to use caries risk as a quality tool is to simply put a goal on decreasing the percentage of patients considered at high risk for caries within a practice (usually evaluated as new patients, recall patients, and a cumulative analysis). A program can track and evaluate on a quarterly basis with a yearly goal used for achievement.
Quality event coding
Perhaps the future of dental qualitative analysis sits with Quality Event Coding (EVT coding). A quality event is an occurrence or consequence relating to the patient's oral health either as a result of oral health care or habits/behavior that may result in negative outcomes.15 Given a preface of "EVT," there are 106 EVT codes proposed as a dummy code quality assessment. More information on the complete dummy code list can be accessed at: http://www.nnoha.org/nnoha-content/uploads/2014/08/Boynes-PP-NNOHA_Quality_EVT-Coding-Presentation.pdf.
The EVT codes are entered into the electronic dental record via the dummy code process (Figure 1) and selected when an event occurs. At a predetermined period of time, the number and type of EVT codes can be analyzed using the "Electronic Dental Software" report mechanism. The EVT codes can be measured as simply as calculating overall percentage of occurrence, to a more thorough analysis of variables. Several methods of how EVT coding can be used for quality practice translation were presented at the Primary Oral Health Conference in 2014 and include the following examples:15
Sealant placement
A series of EVT codes are dedicated to sealant placement and offer information such as how and when sealants fail. These codes can be analyzed in a manner that provides information that improves practice performance by looking for any commonalities among patients and/or providers.
During this process it was determined that the majority of patients with sealant failure within one year were considered overweight or obese. A conference with providers determined that sealant placement on posterior teeth in overweight patients proved difficult due to field of view and direct access issues. Therefore, the dental program created a protocol that team delivery (four-hand sealant placement) was to be employed when a patient was considered overweight or obese. The change resulted in a 15% increase in sealant retention one year after the protocol was implemented.
Restorative care
EVT codes can be used to determine a variety of information, including annual restorative failure rates. Several studies have determined that annual failure rates between 1% to 3% can be achieved with posterior Class I and Class II restorations on a regular basis.16 To appraise this information for a specific practice, a provider can run a report via a dental software program that can filter results comparing EVT coding and CDT procedure code. The total number of relevant EVT codes reported divided by the total number of restorations placed during the analysis time period calculates the percentage of failure with restorations.
READ MORE |Pedonomics: The new economics of pediatric dentistry
Conclusion
Quality assurance is a progression of steps that should lead to practice and performance enhancement. The dental profession currently lacks universality and acceptance of a total quality improvement policy. Several new methods and protocols show great promise in furthering quality assurance in dentistry.
This article focuses on current proposed methodology that offers a quality evaluation process that is more objective. The discussion is framed inside the subject of total quality assurance in dentistry.
References
1. Poorterman JHG, van Weert CM, Eijkman MA. Quality assurance in dentistry: the Dutch approach. International Journal for Quality in Health Care. 1998;10:345-350.
2. Jones ML, Hobson RS, Plasschaert AJM, et al. Quality assurance and benchmarking: an approach for European dental schools. European Journal of Dental Education. 2007;11:137-143.
3. Dental Quality Alliance. Quality Measurement in Dentistry: A Guidebook. American Dental Association, 2012.
4. Bader JD, Shugars DA. Variation, treatment outcomes, and practice guidelines in dental practice. J Dent Educ. 1995;59:61-96.
5. National Maternal and Child Oral Health Resource Center. Safety Net Dental Clinic Manual. Georgetown University, 2010. www.dentalclinicmanual.com [Accessed: 25JAN15].
6. Brennan DS, Spencer AJ. Responsibility loadings for dental services by general dentists. BMC Health Services Research. 2010;10:177.
7. Westerman RF, Hull FM, Bezemer PD, et al. A study of communication between general practitioners and specialists. British Journal of General Practice. 1990;40:445-449.
8. Peck BM, Ubel PA, Roter DL, et al. Do unmet expectations for specific tests, referrals, and new medications reduce patients' satisfaction? Journal of General Internal Medicine. 2004;19: 1080-1087.
9. McGlone P, Watt R, Sheiham A. Evidence based dentistry: an overview of the challenges in changing professional practice. Br Dent J. 2001;190:636-639.
10. Morgan RG. Quality assurance: Quality evaluation of clinical records of a group of general dental practitioners entering a quality assurance program. Br Dent J 2001;191: 436-441.
11. Mascarenhas AK. Patient satisfaction with the comprehensive care model of dental care delivery. J Dent Edu. 2001;65:1266-1271.
12. De St Georges J. How dentists are judged by patients. Dentistry Today. 2004;23:96-98.
13. Pitts NB. Modern concepts of caries measurement. J Dent Res. 2004;83(suppl 1):C43-C47.
14. Ramos-Gomez FJ, Crystal YO, Man Wai NG, et al. Pediatric dental care: Prevention and management protocols based on caries risk assessment. J Calif Dent Assoc. 2010;38:746-761.
15. Boynes SG. Quality Assurance: the New Age of Accountability. Presentation: Primary Oral Health Conference, National Network for Oral Health Access. http://www.nnoha.org/nnoha-content/uploads/2014/08/Boynes-PP-NNOHA_Quality_EVT-Coding-Presentation.pdf [Accessed: 01FEB15].
16. Demarco FF, Correa MB, Cenci MS, et al. Longevity of posterior composite restorations: not only a matter of materials. Dental Materials. 2012;28:87-101.
Sean G. Boynes, DMD, is the director of interprofessional practice at DentaQuest Institute in Charleston, South Carolina. He is also an expert advisor for Safety Net Solutions in Boston, Massachusetts, and a senior dental advisor for CareSouth Carolina in Society Hill, South Carolina. He can be reached at [email protected].