The rise of TMJ disorders and orofacial pain in both patients and dentists has increased significantly during these very stressful and trying times. The September 18th American Dental Association (ADA) Morning Huddle quoted an article in Cleveland’s the Plain Dealer reporting that dentists are seeing more patients who are grinding their teeth, which is probably due to pandemic-induced stress.1
Then, on September 28, the ADA News reported that the ADA Health Policy Institute’s latest poll shows that “a majority of participating dentists have seen a rise in stress-related oral health conditions in their patients since the onset of the COVID-19 pandemic.” More than half of the dentists polled the week of September 21 “reported increases in the prevalence of bruxism (59.4%), chipped and cracked teeth (53.4%), and temporomandibular disorder symptoms (53.4%) among their patients.”2
Stress, clenching, bruxism, and TMJ syndrome are nothing new, but they have most certainly been exacerbated by the pandemic. When patients present with these complaints, most dentists will try to treat them by making a “bruxism” appliance. It has been my experience that most dentists do not realize the patient’s airway should be their concern. Some of you may have just raised your eyebrows and are wondering, “What does this have to do with the patient’s airway?”
Standard of care
If you want to successfully treat clenching, bruxism, TMD, and orofacial pain, the standard of care today is to perform an airway and obstructive sleep apnea (OSA) screening and examination. Nearly every postgraduate orofacial pain residency incorporates dental sleep medicine into their curriculum.
This connection is the primary reason that dentists need to be trained in the areas of bruxism therapy and dental sleep medicine together before they make another “bruxism” appliance. OSA is a medical condition that affects at least 54 million people in the United States, of which 90% is undiagnosed.3 Simply put, OSA is a condition in which the patient stops breathing at night for periods of 10 seconds or more due to an anatomical obstruction of the airway. This can happen tens or hundreds of times a night. OSA is comorbid and dramatically increases the incidence and severity of diabetes, hypertension, stroke, and heart attacks in patients (and let’s not forget that dentists are patients too).
Sleep bruxism
Bruxism is the mechanism the body uses to advance the mandible forward to open the airway so the patient can breathe. Sleep bruxism is much more often the result of an airway issue than it is an occlusal issue. Now, imagine that you make the patient a “bruxism” appliance, and the patient has OSA. The appliance may be pushing the patient’s mandible backwards, thereby closing their airway even more. You have now just made their obstructive sleep apnea worse (effectively choking your patients), and at the same time increased their sleep bruxism.
Dentists also should routinely be testing their patients for both bruxism and OSA, or at the very least, before they make any patient another appliance. This is now possible with a cost-effective home bruxism and sleep monitor, StatDDS, that can quantify the patient’s bruxism episodes index (BEI) and apnea-hypopnea index (AHI), which score how many episodes of bruxism and apneas the patient has for every sleep hour. If you don’t know what these terms mean, you need to get trained.
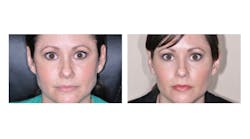
In this way, we can have objective evidence and the data necessary to see how often and at what intensity the bruxism really is. We can also see if the bruxism is related to OSA or if it is primary bruxism. This information is essential and now considered medically necessary before you put anything into the patient’s mouth that can affect the airway. These diagnostics will help guide your treatment with Botox to reduce the contraction intensity of the masseter and temporalis muscles to control sleep bruxism, TMJ/orofacial pain, and facial esthetics (figure 1).
Training is essential in the areas of TMJ/orofacial pain trigger point therapy, dental and facial esthetics, dental sleep medicine, and oral appliances for bruxism therapy before a dentist ever makes another “bruxism” appliance again. Successful restorative, bruxism, and orofacial pain treatments have now entered a new era with the use of cost-effective qualitative testing, Botox, and the relationship of oral appliances and OSA. This will reduce your stress and your patients’ stress by being able to diagnose and more effectively treatment plan for the best therapeutic pain and restorative outcomes.
References
- Oatman A. Dentists see surge in teeth grinding due to pandemic-induced stress. The Plain Dealer. September 16, 2020. https://www.cleveland.com/news/2020/09/dentist-see-surge-in-teeth-grinding-due-to-pandemic-induced-stress.html
- Versaci MB. HPI poll: Dentists see increase in patients’ stress-related oral health conditions. ADA News. September 28, 2020. https://www.ada.org/en/publications/ada-news/2020-archive/september/hpi-poll-dentists-see-increase-in-patients-stress-related-oral-health-conditions
- Obstructive sleep apnea. American Academy of Dental Sleep Medicine. Updated September 19, 2019. https://www.aadsm.org/obstructive_sleep_apnea.php
LOUIS MALCMACHER, DDS, MAGD, is a practicing general dentist and an internationally known lecturer and author. He is the president of the American Academy of Facial Esthetics (AAFE). You can contact him at (800) 952-0521 or [email protected]. Go to facialesthetics.org for information about live-patient Botox and dermal fillers training, solid-filler PDO thread lifts, frontline TMJ and orofacial pain training, dental sleep medicine, bruxism therapy and medical insurance, and to sign up for a free monthly e-newsletter.