Real-world biomimetic dentistry: Cases and the associated economics
Many dentists realize the value of biomimetic dentistry but are unsure how to practically apply it to clinical practice. Biomimetic concepts permeate all aspects of dentistry, from resin infiltration to deep margin elevation, or restoration of teeth with undermined cusps. I’ll share some practical tips that demonstrate not only a biomimetic approach to restorative dental care, but the economic impacts of such therapies.
Diagnosis must precede care recommendations. In addition to proper radiographs, intraoral scan, and clinical exam, I highly recommend dentists take comprehensive, quality dental photographs for documentation, diagnosis, communication, monitoring, and follow-up. This allows them to evaluate patients’ dental conditions on their own time, and also provides legal protection.
You might also be interested in
Biomimetic restorative dentistry (BRD) from the depths of your heart
The biomimetically driven restorative dental practice
Case 1
A 27-year-old patient was referred to me due to discomfort associated with dentinal hypersensitivity secondary to erosion on his posterior teeth (figure 1 above: Initial presentation. Note the exposed dentin due to erosion). His former dentist suggested crown lengthening due to inadequate space for full-coverage crowns.
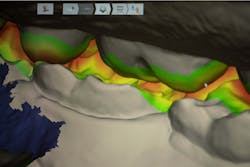
After a thorough evaluation of his clinical presentation, radiographs, and intraoral scan, it was evident that the discomfort was due to exposed dentin. The intraoral scan confirmed there was adequate interocclusal space to restore the eroded tooth structure with a minimally invasive approach (figure 2). All options were reviewed with the patient, and it was mutually agreed upon to address his chief complaint in this manner. Proper isolation is critical for reliable bonding.
Caries lesions were removed and air abrasion was employed to remove impurities on the unprepared tooth surfaces and create increased surface area for bonding. Preparation of the class II carious lesions revealed demineralization on the adjacent tooth structure (figure 3). When lesions such as these are discovered, dentists are often at a crossroads whether to intervene or monitor the area for progression. It is my experience that these early caries lesions can be predictably arrested with resin infiltration (figure 4), and that no intervention usually results in the progression of caries.
In this case, lateral access was achieved by the preparation of the adjacent teeth as part of the proposed treatment plan. Early caries lesions that are noted on radiographs that are not accessible in cases such as this one can be accessed by placing an orthodontic spacer. This patient was restored with direct composite bonding (figure 5) and these restorations have proven to have a favorable long-term outcome (figure 6).
The economic factors of this case
This patient did not have the burden of the cost, or the loss of precious tooth structure during invasive procedures, including crown lengthening and full coverage restorations. This was economically and emotionally favorable for the patient. He opted to have his early caries lesions treated with resin infiltration during this procedure, which created a more productive dental appointment while promoting more favorable long-term health.
Case 2
A 25-year-old female presented with pain on a lower molar (figure 7). Extensive caries was noted, and caries removal was suggested to assess restorability of the tooth and the condition of the pulp, and to formulate a definitive treatment plan. Caries removal did not result in a pulp exposure, but the preparation extended subgingivally.
Since a significant amount of supportive tooth structure remained, it was mutually agreed upon that the tooth would be treated with deep margin elevation, and tooth no. 19 would receive a direct composite restoration on the mesial surface via lateral access to preserve the mesial marginal ridge (figure 8). Isolation is critical in the success of margin elevation, as any contamination of saliva or blood could negatively impact the bonding process and the longevity of the restoration.
A goal of margin elevation is restoring the tooth with contours and emergence profile as close as possible to ideal. Once isolation is achieved, it is necessary to place a matrix that seals the gingival aspect of the preparation and mimics natural contours. The key to achieving this is to place the wedge and the sectional matrix ring without a wedge (figure 9). The preparation extends gingival to the interproximal contact and wedge placement often results in either a flat or concave emergence.
This can promote food or biofilm impaction, discomfort, or periodontal inflammation. Once the gingival aspect of the tooth is restored, the rest of the tooth can be restored as a traditional class II composite restoration (figure 10), or in some cases, an indirect restoration. These teeth were treated using a biomimetic approach (figure 11), which preserved tooth structure and had a favorable outcome (figure 12).
Economic factors for this case
This patient was able to be treated with deep margin elevation and two class II composite restorations. While many third-party payers do not reimburse sufficiently for the time this procedure requires, it was in the best interest of the patient to take this approach.
This patient left the practice and had another deep class II restoration treated on an upper right molar by her “in-network” provider. Insufficient isolation was employed and the use of a wedge at the most gingival aspect of the restoration resulted in a concave contour (figure 13). When the patient returned to my office, she had acute pain, which led to a diagnosis of irreversible pulpitis by an endodontist.
The patient ended up requiring RCT and an indirect restoration on this tooth, with another deep margin elevation to avoid periodontal crown lengthening (figure 14). While I cannot say with certainty that this could have been prevented, I speculate that if proper isolation and contours were achieved, the tooth on the upper right could have had a favorable restorative outcome using a more conservative and economical direct composite restoration, similar to the tooth presented. Moreover, the costs associated in treating the tooth a second time far outweighed the initial investment of a class II restoration using biomimetic principles.
There are many aspects to biomimetic dentistry, and this article illustrates two cases. Here are a few points of emphasis when practicing biomimetic dentistry:
- Documentation and careful diagnosis: When restoring teeth to their natural form and contour, use materials with properties similar to enamel and dentin. Understanding the causative factors of tooth destruction aid in the predictability of tooth rehabilitation.
- Adopting meticulous bonding protocols: Bonding to enamel and dentin is reliable and predictable when performed under ideal conditions. This includes employing proper isolation and handling of all restorative materials.
- Do not create obstacles for meticulous follow-up: When performing prepless occlusal restorations (including sealants), consider using a translucent composite so any changes in the tooth surface beneath the restoration can be identified as early as possible. Moreover, using radiolucent indirect materials aids the dentist in visualizing the tooth’s condition under the restoration, and changes can be identified sooner.
In addition to performing this level of clinical care, dentists should be reimbursed for these efforts. This “less is more” approach often commands more time, paraphernalia (including high-powered loupes or a dental microscope, electric handpieces, and photography equipment), materials, skill, and education.
If a restoration requires more time, materials, and in some cases, multiple appointments to complete, compensation should be concomitant with the requirements of completing the task. Many dental practices that rely on third-party payers may not find this type of care will sustain a dental practice. A business model that prioritizes biomimetic dentistry often encompasses a high percentage of fee-for-service or private pay clients.
Editor's note: This article appeared in the February 2024 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
Abdi Sameni, DDS, FACD, is a former adjunct professor of dentistry and a 1991 graduate of Herman Ostrow School of Dentistry at USC. He is a former faculty for the esthetic selective, which emphasizes a biomimetic approach to restorative care. He was the original director of the USC Advanced Esthetic Dentistry Continuum for the portion relating to indirect porcelain veneers, and he’s the former chairman of the USC International Restorative Dentistry Symposium. He also founded the Los Angeles Dental Symposium.
About the Author

Abdi Sameni, DDS, FACD
Abdi Sameni, DDS, FACD, is a former Adjunct Clinical Associate Professor of Dentistry and a 1991 graduate of Herman Ostrow School of Dentistry at USC. He is a former faculty for the esthetic selective, which emphasizes a biomimetic approach to restorative care. He was the original director of the USC Advanced Esthetic Dentistry Continuum for the portion relating to indirect porcelain veneers, and he’s the former chairman of the USC International Restorative Dentistry Symposium. He also founded the Los Angeles Dental Symposium.