Why are some zirconia crowns failing?
Each month, Dr. Gordon Christensen answers a question from readers about everyday dentistry.
Q: A disturbing number of patients come into my practice with zirconia crowns that are prematurely failing and have not been serving for long. The crowns are coming off tooth preparations, some of which have caries on their margins, and they are not in proper occlusion. They are usually too short, the ceramic is cracking or breaking, the color is incorrect, and many have open contact areas. My colleagues are reporting the same frustrating situations. Why am I seeing these problems with zirconia crowns?
A: Many of us are also seeing the challenges you stated. In my opinion, there are some identifiable reasons. In my answer to you, I will describe the apparent reasons for zirconia crown failure and suggest some potential solutions.
Dental education
The level of education and clinical experience of some new dentists are major challenges. The current large body of knowledge in dentistry does not allow for as much detail or as many hours of clinical time as in the past. Some new dentists graduate with minimal education and superficial clinical experience in many areas of dentistry. The result is they require years of practice and significant continuing education to become clinically competent. If you are a new dentist, please get some pragmatic, hands-on clinical education in the areas in which you feel weak as soon as possible.
Zirconia crowns in dentistry: Uses, clinical challenges, and solutions
Tooth preparations
This subject is probably the most important and predominant problem. Almost all dentists have been taught proper crown preparation characteristics in dental school. However, if you look at impressions of tooth preparations dentists send to laboratories, you would see that there is a significant problem. Many tooth preparations do not satisfy the known characteristics that provide adequate retention, strength, and long-term wear resistance.
Also by Dr. Christensen:
Which crown types are best for what situations?
Most research information on crown preps states that an adequate tooth preparation has axial walls that extend 4 mm from the gingival margin to the occlusal table, and that the axial walls should be 20 degrees or less from the long axis of the tooth preparation. The depth of the marginal chamfer for a zirconia crown should be about 0.6 mm minimum for optimum strength. The occlusal reduction for a zirconia crown should be at least 1.5 mm or more to allow adequate strength of restorative material and optimum occlusal spacing of the crown occlusal contacts to produce a crown that is not too high when seated (figure 1).
Some labs are spacing the crown occlusal surfaces up to 500 microns (0.5 mm) out of contact to ensure you will not have to adjust the crown. This is far too much and places trauma on the adjacent tooth until the opposing and crowned teeth have extruded. Ideally, crowns should have perfect occlusion, but that is not likely. They should be spaced out of occlusion only a few microns to allow rapid tooth extrusion in a few days or a maximum of weeks. Seldom do you see these characteristics. Of course, sometimes tooth size and shape do not allow optimum preparations, but most of the time an optimum prep is possible.
What can be done to salvage a crown that has come off during service due to an inadequate prep?
At seating, either originally or after coming off in service, make diamond scratches on the external wall surfaces of the prep and on the internal axial surfaces of the crown. Seat with a resin cement, such as RelyX Unicem 2 (3M ESPE) or Maxcem Elite Chroma (Kerr). In near-impossible cases that lack retention, use C&B Metabond Quick (Parkell).
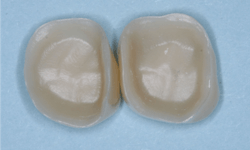
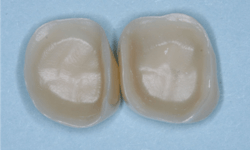
Luting characteristics on internal crown and external prep surfaces
The internal surfaces of current zirconia crowns are usually very smooth (figure 2). If the prep is adequate as described, this is usually not a problem. If there is any question about the potential zirconia crown retention, roughen the internal surfaces of the crown with a coarse diamond. If you do this, make sure you use a 3Y class 5 ceramic material. Many zirconia brands have modified material formulas that will not tolerate adjustment with a coarse diamond and will break. Similarly, roughen the external axial walls of the inadequate tooth preparation.
All brands of the most popular cement types are either resin or resin-modified glass ionomer. They are resilient! Lack of luting irregularities on the internal surfaces of the prep and the crown may allow the crowns to come off during service because the cement is resilient.
Caries on crown margins
Current crown margins are not the tight margins that were available with the gold restorations of the past. Regardless of the ceramic material used, the margins are usually open about 60 microns (0.06 mm) or more.
Additionally, dental lab technicians verify that the majority of impressions (both conventional and virtual) that are coming to American labs are inadequate and do not show all of the gingival margins. Make sure the cements you use are adequately radiopaque so you can differentiate whether a margin is faulty or that the radiographic void is just cement. Some cements are too radiolucent. In almost all categories of materials, the products from Ivoclar Vivadent are the most radiopaque on the current market and should be used if you have a questionable margin.
If you know the margins are not fitting adequately or the patient has highly active caries, use a cariostatic resin-modified glass ionomer cement—not a resin cement. Examples are RelyX Luting Cement (3M), Fuji Plus (GC America), or FujiCem (GC America).
When caries occurs on a crown margin and a margin repair is being accomplished, there are several new materials that provide optimum fluoride release for the repair as proven by the Technologies in Restoratives and Caries Research (TRAC) Division of Clinicians Report Foundation. Among the most fluoride-releasing materials currently available are Equia Forte (GC America) and Ketac Universal (3M).
Open contact areas
Contact areas should be broad and flat to prevent food impaction. Leaving a contact area open is almost a sure invitation for caries to form (figure 3). Suggest to your lab that you want broad, flat, tight contact areas on your crowns. It is far easier to reduce a contact area than to add to a deficient one. The lab technician can meet most of these characteristics easily by adjusting the computer setting for the contact area.
If the patient has tooth mobility, tell the lab technician to make the contacts very tight, and then adjust them in the mouth if necessary.
Color of zirconia crowns
Obtaining optimum color for zirconia crowns has been a near impossibility (figure 4). Almost all zirconia crowns come back to you a shade or two too light. If you require low-cost zirconia crowns from your lab, you have only one choice—have the crowns made one or two shades darker than the shade guide color you selected. If you want 3Y class 5 (the original formulation) zirconia crowns that actually have the correct color, you will pay significantly more (figure 5).
The 3Y zirconia can be internally stained at the presintered stage to achieve the color you desire after sintering.
New formulations of zirconia are coming on the market rapidly; for these, companies are not using the original zirconia formulation. Some of the crowns look more esthetically pleasing than the original zirconia formulation, but they have lower strength and need long-term research to validate their formulations.
Zirconia is not zirconia
The original BruxZir (Glidewell) 3Y zirconia (3 molar percent yttrium oxide content) has enormous strength and a property called transformation toughening (not allowing crack propagation). These characteristics have made the 3Y zirconia almost indestructible. Clinicians Report Foundation (TRAC division) studies over nearly 10 years on 3Y single zirconia crowns have shown almost no failures. Some of the new “esthetic” zirconia brands with modified formulations have reduced strength and little or no transformation toughening.
Ask your lab technician what type of zirconia they are using. They should know the answer to that question. If they do not, find another lab that does know what they are using.
A conservative suggestion to you relative to zirconia crowns is to use the original 3Y formulation of zirconia until such time has elapsed to validate the adequacy of a new brand of zirconia, or be willing to accept failure in the event that it occurs.
Summary
Unfortunately, the current acceptability of many so-called zirconia crowns could be better because of differences in zirconia formulations. Zirconia is not zirconia. I have discussed the most frequently occurring challenges with these crowns. Most of the problems can be avoided by using the potential solutions described in this article for each of the identifiable challenges.
Zirconia is here. It is not going away. As such, it is our professional responsibility to understand it better and use it to an optimum level.
Author’s note: The following educational materials from Practical Clinical Courses will offer you and your staff more insight on the topic of this question.
One-hour videos
• Foolproof, Fast Single-Crown Procedure (Item V1980)
• Rescuing Failing Fixed Prosthodontic and Direct Restorations (Item V1992)
Two-day hands-on courses
• Faster, Easier, Higher-Quality Dentistry with Dr. Gordon Christensen
• Restorative Dentistry 1—Restorative, Esthetic, Preventive with Dr. Gordon Christensen
For more information about these educational products, call (800) 223-6569 or visit pccdental.com.
Editor's note: Originally published in 2019; updated in 2022.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.