Winner in prevention: The GBT experience
Guided Biofilm Therapy (GBT) is a systematic, evidence-based, modular concept for professional prevention and periodontal and peri-implant treatment for lifelong maintenance. A unique global survey of over 400,000 patients provided a clear result: more than 94% preferred GBT over traditional methods as a positive overall experience.
Oral health is based on two pillars: firstly, the professional removal of biofilm and dental calculus in conjunction with intensive oral hygiene education, and secondly, sound advice and motivation for oral health.1-3
Both pillars have a preventive effect on both oral and general health, as well as on their interaction. However, many patients receive regular preventive dental care only if the experience is a positive one and they are involved in the preventive treatment as a responsible partner.4,5
The EMS Dental concept of Guided Biofilm Therapy developed by universities and dental practitioners fulfills all these requirements.6,7 The current results of a worldwide patient survey in dental practices that work according to the state-of-the-art GBT method are presented here.
Conclusive results
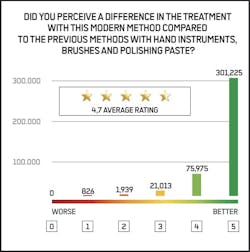
Since the fall of 2021, GBT-certified practices and clinics have been receiving completed questionnaires by their patients for anonymized evaluation (n=400,978, as of November 4, 2024). These comprise seven questions to be rated on a scale of 0 to 5. All responses demonstrated a high level of acceptance for GBT (93.4%-94.6%) with approximately 4.7 out of 5.0 possible points. In a direct comparison of GBT with previous methods (hand instruments, brushes, and polishing pastes), 94.1% preferred the GBT protocol (figure 1). Corresponding results were obtained with 93.6% for the average assessment of freedom from pain.
The vast majority (93.4%) also considered the disclosure of biofilm, an integral part of GBT, to be useful. It is used by the dental hygienist as quality control to ensure that the biofilm has been completely removed and also provides patients with a basis for improved oral hygiene. To offer GBT treatment at the highest level, it is a prerequisite that the practice team receive theoretical and practical training from the Swiss Dental Academy (SDA) of EMS.
Optimal preservation of tooth structure
The professional removal of plaque must be effective and as time-saving as possible; however, tooth enamel, dentin, and root surfaces should be treated with maximum care, even when plaque is removed repeatedly over a long period of time, to avoid loss of tooth structure.8,9
Loud noises, such as that from ultrasonic instruments and unpleasant scratching with hand instruments, should be avoided as much as possible. Guided Biofilm Therapy as a clinical protocol fulfills these conditions in a well-documented scientific manner. During professional mechanical plaque removal, the biofilm is first removed as the causative factor with air-flowing from all accessible oral surfaces.10 This can be achieved most effectively and economically using the AIRFLOW Prophylaxis Master device in combination with the AIRFLOW MAX or the PERIOFLOW handpiece and with the use of AIRFLOW PLUS powder (figures 2 and 3).11
Only in the second step is a piezoceramic ultrasonic scaler (PIEZON PS NO PAIN) used to remove the now more visible residual dental calculus. Both technologies are particularly gentle on tissue and are rated by patients as being more pleasant than other instruments.12,13 Based on a positive overall treatment experience, patients are motivated to return for regular recall appointments. Subsequent polishing with rubber cups and paste does not improve surface smoothness and therefore provides no additional benefit.9,14
The GBT experience
Patients desire effective prevention utilizing state-of-the-art science and technology. To ensure patient loyalty-and thus the economic success of a dental practice-it is crucial to provide preventive treatment that is painless, structured, and relaxed while maximizing efficiency: the GBT experience. The dental team also benefits from the systematic concept and ergonomically optimized devices and techniques. According to unanimous user feedback, these features help avoid excessive workloads caused by the daily, time-consuming use of hand instruments.15
The results of the survey presented here, involving more than 400,000 patients from dental practices that routinely employ GBT, demonstrate the method’s high level of acceptance in everyday clinical practice. These findings confirm study data from the University of Zurich, where 96% of surveyed patients expressed a preference for GBT over traditional methods involving hand instruments and polishers.16 Guided Biofilm Therapy remains the absolute favorite for professional prevention among patients.
GBT certification: The best investment for your practice
Professional prevention at the highest level not only enhances the clinical qualifications of your team but also significantly improves the economic efficiency of your practice. GBT certification ensures standardized clinical and technical quality, backed by the Swiss Dental Academy of EMS.
For more information, visit ems-dental.com.
Editor’s note: First published in ZMK. 2024;40(11-12):684-685. Spitta GmbH. Reprinted with permission.
References
1. Axelsson P, Nyström B, Lindhe J. The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J Clin Periodontol. 2004;31(9):749-757. doi: 10.1111/j.1600-051X.2004.00563.x
2. Tonetti MS, Chapple IL, Jepsen S, Sanz M. Primary and secondary prevention of periodontal and peri-implant diseases: Introduction to, and objectives of the 11th European Workshop on Periodontology consensus conference. J Clin Periodontol. 2015;42 Suppl 16:S1-4. doi: 10.1111/jcpe.12382
3. Herrera D, Sanz M, Shapira L, et al. Periodontal diseases and cardiovascular diseases, diabetes, and respiratory diseases: summary of the consensus report by the European Federation of Periodontology and WONCA Europe. Eur J Gen Pract. 2024;30(1):2320120. doi: 10.1080/13814788.2024.2320120
4. Amerio E, Mainas G, Petrova D, et al. Compliance with supportive periodontal/peri-implant therapy: a systematic review. J Clin Periodontol. 2020;47(1):81-100. doi: 10.1111/jcpe.13204
5. Enkling N, Marwinski G, Jöhren P. Dental anxiety in a representative sample of residents of a large German city. Clin Oral Investig. 2006;10(1):84-91. doi: 10.1007/s00784-006-0035-6
6. Bastendorf KD, Strafela-Bastendorf N. Auf das klinische Protokoll kommt es an - PZR, UPT und GBT. Quintessenz. 2020;71(12):1380-1389. https://www.quintessence-publishing.com/deu/de/article/867027/quintessenz-zahnmedizin/2020/12/auf-das-klinische-protokoll-kommt-es-an-pzr-upt-und-gbt
7. Lang N, Lussi A, Bastendorf KD. Wissenschaftlicher Konsensus Guided Biofilm Therapy-Protokoll. Ein neues Konzept für die primäre und sekundäre Prävention. EMS Electro Medical Systems. 2019.
8. Camboni S, Donnet M. Tooth surface comparison after air polishing and rubber cup: a scanning electron microscopy study. J Clin Dent. 2016;27(1):13-18. https://www.ncbi.nlm.nih.gov/pubmed/28390211
9. Graetz C, Plaumann A, Wittich R, et al. Removal of simulated biofilm: an evaluation of the effect on root surfaces roughness after scaling. Clin Oral Investig. 2017;21(4):1021-1028. doi: 10.1007/s00784-016-1861-9.
10. Mensi M, Scotti E, Sordillo A, et al. Plaque disclosing agent as a guide for professional biofilm removal: a randomized controlled clinical trial. Int J Dent Hyg. 2020;18(3):285-294. doi: 10.1111/idh.12442
11. Donnet M, Fournier M, Schmidlin PR, Lussi A. A novel method to measure the powder consumption of dental air-polishing devices. Appl Sci. 2021;11(3):1101. doi: 10.3390/app11031101
12. Bühler J, Amato M, Weiger R, et al. A systematic review on the patient perception of periodontal treatment using air polishing devices. Int J Dent Hyg. 2016;14(1):4-14. doi: 10.1111/idh.12119
13. Aslund M, Suvan J, Moles DR, et al. Effects of two different methods of non-surgical periodontal therapy on patient perception of pain and quality of life: a randomized controlled clinical trial. J Periodontol. 2008;79(6):1031-1040. doi: 10.1902/jop.2008.070394
14. Kruse AB, Fortmeier S, Vach K, et al. Impact of air-polishing using erythritol on surface roughness and substance loss in dental hard tissue: an ex vivo study. PLoS One. 2024;19(2):e0286672. doi: 10.1371/journal.pone.0286672
15. Dong H, Barr A, Loomer P, et al. The effects of periodontal instrument handle design on hand muscle load and pinch force. J Am Dent Assoc. 2006;137(8):1123-1130; quiz 1170. doi: 10.14219/jada.archive.2006.0352.
16. Furrer C, Bättig R, Votta I, Bastendorf KD, Schmidlin PR. Patientenakzeptanz nach Umstellung auf «Guided Biofilm Therapy» [Patient acceptance of «Guided Biofilm Therapy»]. Swiss Dent J. 2021;131(3):229-234. German. doi: 10.61872/sdj-2021-03-02
GBT certification: The best investment for your practice
Professional prevention at the highest level adds significant advantages to the clinical qualifications of the team, but also to the economic efficiency of the practice. This is assured by GBT certification, with standardized clinical and technical quality assured by the Swiss Dental Academy of EMS.
More information available at
https://gbt-dental.com/PF-ZMK1224-DE
About the Author

Dr. med. dent. Jan Hermann Koch
Dr. med. dent. Jan Hermann Koch is a practicing dentist in Freising, Germany, focusing on conservative dentistry, pediatric dentistry, and periodontology. He has more than 20 years of experience as an editor, independent journalist, and public relations professional. He received his dental degree from the University of Berlin and is a member of the Bavarian Dental Association and the German Association of Oral and Maxillofacial Medicine.
Updated January 25, 2024