Two drugs, lidocaine HCl 2% with epinephrine and articaine HCl 4% with epinephrine, comprise more than 90% of the injectable dental anesthetic market and have represented the state of the art for decades.1 For pharmacological reasons, both drugs must be stored in a highly acidic solution (pH 2.9), which creates several problems, including a burning sensation upon injection and delayed onset of anesthesia.
Neutralizing the acid prior to injection by mixing sodium bicarbonate with the drugs is called “buffering” and has been shown to eliminate both the sting and the latency, reduce toxicity, and increase reliability in inflamed tissue.2–4
Dentists need a faster-acting anesthetic
Will the new personal protective equipment (PPE) requirements change the way we think about administering dental anesthetic and make buffering more popular? Because of the delay in anesthetic onset, and to avoid wasting time, most dentists have adopted the practice of injecting anesthetic and then leaving the room to work on another patient while waiting for the anesthesia to take effect, but recent events make the economics of this protocol questionable. The Centers for Disease Control and Prevention and Occupational Safety and Health Administration now recommend that dental personnel don new PPE for each patient and not wear that PPE outside the operating room to avoid the spread of contagious diseases.5 Dental offices will soon look more like hospitals and be forced to adopt similar contamination protocols.
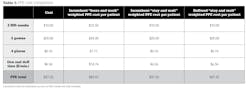
Under the new guidelines, the “leave and work” strategy now requires two changes of very expensive PPE—or three, if anesthesia fails (table 1).
Ideally, dentists should stay with the patient after injecting anesthetic, but because of the delay in onset and unreliability associated with the current (“incumbent”) drugs, this costs an average of $60.35 per patient in lost time (table 2).
Fast-acting buffered drugs (e.g., Anutra or Onpharma Onset) can reduce the time cost of staying in the room to $12.79, saving $47.56 per patient.
Patients want a less painful injection
Would a better injection experience be worth the extra cost of buffering to patients? Recent polling data developed by Balanced pHarma, a pharmaceutical company in Charlotte, North Carolina, shows that 51% of patients believe the injection is the most fearful thing about visiting the dentist, and 47% said that a painless injection was a “must have” when selecting a dentist.6 More than half said they would pay at least 10% extra for a procedure if the dentist used a less painful anesthetic, and 36% said they would change dentists if their current dentist didn’t use a less painful anesthetic if it were available.6
If these polling data are correct, then a less painful anesthetic would help more people overcome their dental fears and bring a significant marketing advantage to typical dental practices.
Overall buffered anesthetic value
After adding the additional product cost and subtracting the PPE savings, buffering could either cost an additional $7.43 or save as much as $26.02, depending upon the product. Dentists will have to decide whether the new PPE costs and added patient comfort have tipped the economic scales in favor of buffered anesthetics.
Current and future buffering options
Buffered anesthetic is not presently available in standard dental cartridges, but there are currently three methods to compound it in the dentist’s office and two new drugs in development. At present, two commercially available mixing devices are sold by Anutra7 and OnPharma,8 and there is also the “do it yourself” method,9 which involves injecting bicarb solution into the dental cartridge using a tuberculin syringe. On the horizon, Balanced pHarma is seeking Food and Drug Administration approval for its developmental drug Libracaine. This drug will essentially be buffered versions of both lidocaine and articaine provided in standard dental cartridges. Availability is expected in the very near future.
References
1. Malamed SF, Tavana S, Falkel M. Faster onset and more comfortable injection with alkalinized 2% lidocaine with epinephrine 1:100,000. Comp Cont Edu Dent. 2013;34(2):10-20.
2. Guo J, Yin K, Roges R, Enciso R. Efficacy of sodium bicarbonate buffered versus non-buffered lidocaine with epinephrine in inferior alveolar nerve block: A meta-analysis. Dent Anesth Pain Med. 2018;18(3):129-142.
3. Warren VT, Fisher AG, Rivera EM, et al. Buffered 1% lidocaine with epinephrine Is as effective as non-buffered 2% lidocaine with epinephrine for mandibular nerve block. J Oral Surg. 2017;1363-1366. doi:10.1016/j.joms.2016.12.045
4. Kattan S, Lee Su-Min, Karabucak B. Do buffered local anesthetics provide more successful anesthesia than nonbuffered solutions in patients with pulpally involved teeth requiring dental therapy? J Am Dent Assoc. 2019;150(3):165-177.
5. Dentistry workers and employers. OSHA. https://www.osha.gov/SLTC/covid-19/dentistry.html
6. Intoducing pH-balanced Libracaine. Balanced Pharma. https://balancedpharma.com/meeting-a-medical-need/may-2020-survey
7. The new dental workflow. Antura Medical. https://anutramedical.com/
8. Onset Buffering System. Onpharma. https://onpharma.com/
9. Goodchild JH, Donaldson M. Novel direct injection chairside buffering technique for local anesthetic use in dentistry. Comp Contin Educ Dent. 2019;40(7):e1-e10
JOHN SCOTT KEADLE, DDS, is a practicing general dentist and the owner of New Smile Carolina in Charlotte, North Carolina. He is the founder and chief medical officer of Balanced pHarma, a pharmaceutical company whose mission is to make local anesthesia faster and less painful, and the developer of Libracaine, a buffered local anesthetic product. Dr. Keadle graduated from West Virginia University Dental School in 1989 and can be reached at [email protected].