Economically and clinically leveraging implantology in your solo practice, DSO, or DDSO: Innovations in immediate implants
Calvin Bessonet, DDS
Michael A. Sisk, DDS
Introduction by Michael A. Sisk, DDS
DURING the last few years, some of the greatest innovations in implant designs have occurred in relation to the immediate placement of implants. “Old-school” implant designs generally involved cylindrical, nontapered implant bodies with relatively dull and shallow threads. But modern, more recent implant designs have included tapered implant bodies with sharper, deeper, and more aggressive threads. This has allowed for more engagement in the bone (osseocompatibility), with greater primary stability, which has equated to earlier loading times. These more modern designs have also created greater success rates, which has led to the immediate implant procedure being more popular with general practitioners in the United States.
By the end of this article series, it is our goal that you have a clear pathway to lower overhead, greater profitability, a vision for the investment side of dentistry, and a renewed passion for the deeper levels of the implant side of your practice—particularly through the immediate implant procedure.
For dentists who currently do not place implants, the barriers to providing this service to an ever-increasing population who needs and demands implant services are twofold. First, the cost for a solo private practitioner to invest in the equipment, inventory, instruments, and supplies necessary to place implants safely and effectively can be difficult to calculate. Second, the cost and the length of time required for training can be prohibitive. Training requires time away from the practice and a sizable financial commitment to achieve expert status. Together, these barriers can prevent many dentists from ever getting started.
Today, many dentists are forming private practice groups known as dentist-owned dental service organizations, or DDSOs. From a single location to a large group of offices and owners, these private dentists essentially develop cooperatives for mutual benefits so that they may continue to offer services on a personalized basis and share in some advantages generally only reaped by the larger DSOs. Our three-location group, as with others, receives favorable pricing with dental suppliers and manufacturers, such as direct implants through IH Biomedical (around $98 per implant and $41 per abutment). As a group, we are able to significantly reduce the cost of entry to implant dentistry by the savings on implants and components through IH Biomedical’s manufacturer-direct relationships. As a DDSO, we also take advantage of lab savings, lowered equipment costs, and preferred banking relationships, due to the buying power that groups have over individuals.I began my process into deeper levels of investing in dentistry through some of the concepts described in Transition Time by Brady Frank, DDS. This is a book that I believe has the keys to personalizing your own strategic growth plan. One such key for me has been incorporating an institute for continuing education into my private group of three locations. Pennsylvania Implant Institute, in collaboration with several other institutes across the country, provides affordable implant education at novice, intermediate, and advanced levels.
Let this serve as an introduction to commentary by one of the most talented implantologists who I have ever had the pleasure of studying under: Calvin Bessonet, DDS. Dr. Bessonet received much of his advanced implant training through courses offered by Hilt Tatum, DDS, in the Dominican Republic. Dr. Bessonet’s innovative approaches to ridge splitting, lateral window sinus lifts, and full-arch work are impressive. As presented by Dr. Bessonet in the next section, the following immediate implant placement tips have proven to be valuable in my busy group. We see many emergency patients converting to extraction, implant, and graft cases.Commentary by Calvin Bessonet, DDS
Tips for immediate implant placement
One of the best ways to practice economical and predictable implant dentistry is to use, when appropriate, immediate placement at the time of extraction. The patient is in the chair and motivated to complete treatment right then. I have found that, with some patients, if you extract the tooth and wait a few months to place the implant, they will sometimes get used to the empty space and procrastinate on having the tooth replaced. The repercussions of not replacing the tooth, such as bone loss, shifting, bite changes, and occlusal overload of neighboring teeth, take time to manifest and are not always readily apparent to the patient. But once these problems are noticed by the patient, the treatment plan often becomes more involved and expensive—and sometimes out of reach financially. Large grafting procedures can also be intimidating to patients, which prevents them from following through with procedures.
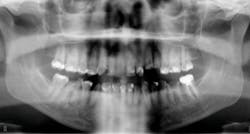
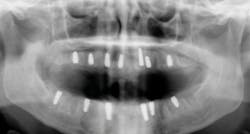
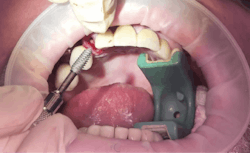
Another reason immediate placement is advantageous is that once the extraction is complete, the hole is usually already in the proper place for the implant. You may have to redirect your osteotomy slightly palatally, mesially, or distally, but the socket serves as an excellent guide for placement. In some cases, especially premolars, you can use an implant with aggressive threads to place without any osteotomy at all. You can engage the mesial and distal walls to achieve primary stability. This greatly shortens the appointment time, lowers risk, and increases patient satisfaction. Figures 1 and 2 show a MorsTorq in site No. 21 that was placed after an atraumatic extraction during my most recent two-day Louisiana Implant Institute course. Note the sharp threading on the MorsTorq, which allows for optimized immediate placement performance.There are some circumstances where immediate placement is not desirable. If the socket is too large to engage the mesial and distal walls and vital anatomical structures are located just apical to the socket, immediate placement is not recommended. Chronically infected sites also present a higher risk for immediate placement. If you can completely rid the socket of all soft tissue and the patient has the appropriate antibiotics onboard, it is possible. However, most of these cases are more predictably treated with early placement (waiting four to six weeks without grafting) or delayed placement (three to six months with grafting).
When placing an immediate implant, you must maintain a gap of at least 2 mm between the implant and buccal wall to prevent resorption of the plate and thread exposure.Next in the series
We certainly hope that you have received some actionable immediate implant placement tips for the benefit of your practice and patients. Stay tuned for part three, which appears next month, as we explore successful private practice models that allow for various implant skill levels among practitioners to be satisfied.
CALVIN BESSONET, DDS, is committed to lifelong learning in the dental field and has been recognized by other general dentists as a leader who exemplifies the importance of quality continuing dental education. He has been placing and restoring implants for more than 15 years.
MICHAEL A. SISK, DDS, graduated from the University of Maryland, Baltimore, College of Dental Surgery. He earned his doctor of dental surgery degree in 1983. He has a love for surgical implant placement and a passion to teach others modern, innovative approaches to implant dentistry.
Editor’s note: This article is part two of a six-part series on how dentists can benefit from the immense changes that implant dentistry has brought to the profession. Part one of this series appeared in June and may be found on dentaleconomics.com. Part three will appear in August.