From clunky to confident: How to streamline dental microscope integration
The dental operating microscope has been in clinical use since the 1990s.1 Despite its longstanding presence, widespread adoption remains limited among general practitioners in the United States and globally.2 Even when the equipment is acquired, stigma and misconceptions about its intended use persist.
Dispelling the endodontics-only myth
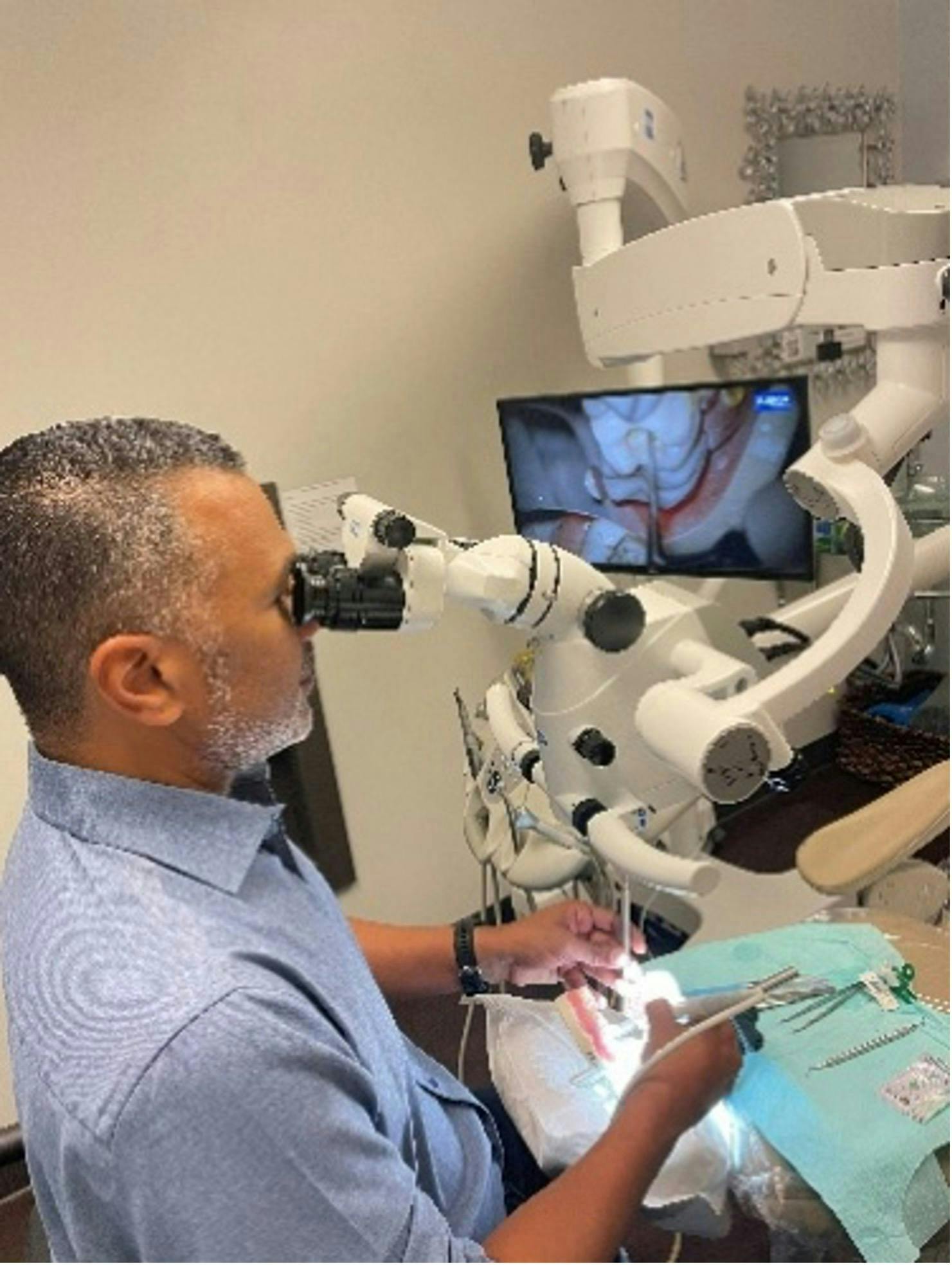
A frequent comment encountered at professional meetings and training sessions—particularly when a dentist or hygienist approaches a microscope demonstration—is, “Oh, this is an endodontic microscope,” or “This is only for endodontics.” Such assumptions reflect a fundamental educational gap or a misinterpretation of the tool's versatility. In reality, the dental microscope is an invaluable resource for all practitioners, irrespective of specialty. Today’s clinical demands—for precision, enhanced visual feedback, and improved operator posture—necessitate broader integration of this technology.3
Productivity concerns and ergonomic consequences
A recurrent critique voiced by dentists, including specialists who own microscopes, is that its use slows them down, decreasing productivity. Consequently, the microscope is often relegated to a corner, unused, or humorously repurposed as a coat rack. Meanwhile, these same professionals frequently suffer from musculoskeletal discomfort and repetitive strain injuries—consequences of poor posture, inefficient team dynamics, and inadequate ergonomic practices.
The importance of training in microscope dentistry
Effective adoption begins with comprehensive training—ideally prior to acquisition. Mastering the essential techniques and ergonomic principles associated with microscope use is vital. Even for those who already own the technology, continued education can yield substantial benefits.4
To overcome the initial slowdown in workflow, clinicians should adopt a structured, incremental approach. Begin with simple cases and gradually progress to more complex ones as confidence and proficiency improve.
Behavioral change stems from habit formation. Learning to identify ineffective habits and replace them with intentional, ergonomically sound practices is a personal and professional undertaking.
Integration requires systematic support
Like all advanced technologies, successful integration of the dental microscope requires consistent training, adherence to established guidelines, and an effective system that supports seamless incorporation into daily workflows. Far from a luxury, the microscope represents a dual investment: enhancing the practitioner’s health and extending career longevity, while simultaneously improving treatment outcomes for patients.
Guidelines for dental microscope integration:
-
Study ergonomic principles specific to microscope use.
-
Enroll in hands-on microscope dentistry immersion programs.
-
Begin with 50% of your clinical time under the microscope; increase usage by 10% each week. Daily use over 4–8 weeks will typically result in 80%–90% microscope usage.
-
Start with simple cases—anterior teeth, bicuspids, or single-tooth procedures—then advance to posterior or multi-tooth cases as skills develop.
-
Emphasize the use of indirect vision.
-
Train assistants in mirror management and four-handed techniques.
-
Follow a systematic approach to ergonomic positioning.
-
Instruct your assistant to observe and assess your posture from a lateral view, providing real-time feedback to help you adjust and refine your technique.
-
Maintain patience, consistency, and purpose in your practice.
Why ergonomics and microscope dentistry go hand in hand
Adaptation and change are inherently difficult, particularly for professionals trained to perform dentistry with unaided vision or traditional loupes. These long-established habits, however, carry risks. As documented in the literature, 60%–80% of dentists and hygienists suffer from musculoskeletal disorders—a call to action that cannot be ignored.5,6
The integration of ergonomics into the dental curriculum, from the pre-clinical stage onward, should be standard. The implementation of ergonomically sound practices and the use of the dental microscope should be foundational, not optional. Pursuing excellence and elevating clinical standards demands the systematic use of the microscope. Yet, without ergonomic application, the microscope alone addresses only part of the problem.
Editor's note: This article originally appeared in DE Weekend, the newsletter that will elevate your Sunday mornings with practical and innovative practice management and clinical content from experts across the field. Subscribe here.
References
- Carr GB, Murgel CA. The use of the operating microscope in endodontics. Dent Clin North Am. 2010;54(2):191-214.
- Selden H. The dental-operating microscope and its slow acceptance. J Endod. 2022;28(3):206-207.
- Perrin P, Neuhaus KW, Lussi A. The operating microscope in dental general practice. Schweiz Monatsschr Zahnmed. 2000;110(9):946-960.
- Ortiz Hugues JC. The dental microscope—not just for endodontics. Decisions in Dentistry. 2024;10(2):8-9.
- Ohlendorf D, Erbe C, Hauck I, et al. Prevalence of musculoskeletal disorders among dentists and dental students in Germany. Int J Environ Res Public Health. 2020;17(23):8740.
- Jain R, Bhaskar DJ, Yadav P, et al. Prevalence of musculoskeletal disorders among dental professionals: an umbrella review. Eur J Gen Dent. 2025;14:1–10.