Multidisciplinary microscope dentistry vs. naked eye dentistry: A stark contrast in precision, accuracy, and quality
Precision is the quality, condition, or fact of being exact and accurate, and accuracy means free from error or defect; consistent with a standard, rule, or mode. If we carefully analyze these two words, it is the standard that our patients expect in our dental procedures, since the long-term prognosis of treatment depends on precision and accuracy.
It is no secret that the demands on a dentist’s vision are high, since we work in narrow areas with diameters that are often microscopic, and in a dark cavity, full of shadows and neighboring structures that interfere with the visual angle of work, like the cheeks and the tongue, where the need for optical aids and high magnification influence visual acuity.1
Conventional naked eye dentistry and even the low magnification of magnifying loupes are not enough to obtain all the information needed to perform precise dental procedures, as details are of utmost importance in dentistry. Shanelec and Tibbets reported that limitation regarding precision of treatment is not in the hands, but in the eyes. Working without magnification, movements as precise as 1–2 mm versus 20× magnfication, the refinement in movements can be as little as 10–20 microns at a time—enough reason to try high magnification in dentistry.2
Another important feature of high-magnification microscope dentistry is the capacity to improve the visual resolution of the human eye, which allows for the ability to detect different entities as individuals, limited to 0.2 mm if they are apart from one another. With a dental microscope, one can distinguish these entities if there is a distance of merely 0.006 mm between them.3
The focal distance from the dentist’s eye to a small area in the mouth promotes a forward-leaning posture to facilitate the perception of intricate details.4 It is impossible to separate the musculoskeletal problems that afflict the dentist from the common working positions resulting from the limitations of the human eye.5 Patients expect quality dental treatment when they book a consultation, so high-precision diagnosis and treatment are critical when it comes to generating optimal results and performance by the dentist. 6
There is a widespread myth among dentists that dental microscopes are exclusively for endodontic treatment. This is nonsense, since the need for light, visualization, communication, and neutral working posture is an absolute requirement for all dental disciplines and specialties.
The accuracy, precision, and details available through dental microscopy are a result of illumination and multiple steps of magnification. Understanding lighting and magnification and the benefits of quality dentistry are important to accomplish better outcomes from every perspective.7
Lighting
To analyze the teeth and identify possible problems, the dentist needs to be able to distinguish small details amidst low contrast in the dark mouth area. To obtain adequate lighting of the mouth, the quality of the light, intensity distribution, and the physical positioning of the light need to be adjusted to the dentist and the patient’s mouth.
The absence of good lighting will result in an inability to see much detail, appearance of afterimages, eyestrain, fatigue, and/or even long-term damage to the dentist’s eyes.8
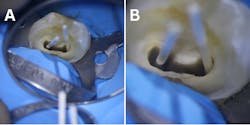
The light from the dental chair is not enough to illuminate the work field; the distance from the lamp to the chair, the power of the light, and the shadows the lamp generates make the light dissipate a lot, losing most of its ability to improve the operator's visual capacity. Even the LED lights on magnifying glasses generate shadows when they reach the oral cavity since they are not coaxially integrated into the lighting system.9 Microscope dentistry, conversely, allows for coaxial lighting which travels in the same axis of vision as the human eye and prevents light from being lost along the way and eliminates shadows that darken the field of vision (figure 1).10
Magnification
Magnification is the process of enlarging the apparent size, not the physical size, of something. This is achieved in the microscope through optical lenses and prisms. The final result of different magnification steps, ranging in modern microscopes from five to six steps, are given by formulas that include the magnification of the binoculars, the magnifying glass, and the focal objective.
Our dexterity depends a lot on the quality of our vision. As we increase magnification, our motor skills become finer, therefore we are able to achieve more precise movements in small spaces. 11 Our margin of error in dental work is limited to microns, which requires visual aid for most treatments. It does not matter if it is a prosthetic, endodontic, or restorative periodontal treatment, the need to see more and better is imminent.
Multiple magnifications allow the operator to jump from low to medium to high magnification steps depending on the visual requirements and specific circumstances. For example, when carving a tooth for dental prosthesis, in-depth circumferential vision is needed, therefore active work with a high-speed piece requires a greater field of view with low magnification, the position of the head of the high- or low-speed piece, the direction of the drill, the axial axis of the tooth, and the parallelism in relation to the active drill, the adjacent soft tissues, neighboring pieces, structures such as the tongue, cheeks and the handling of the mirror among others.12
Understanding the effect of magnification is crucial. Many dental microscopists abuse high magnification steps, depriving themselves of relevant information necessary to execute treatment without interruptions and minimizing errors due to lack of visual field (figure 2).
The higher the magnification the smaller the visual field, but on the other hand, the higher the magnification the less depth of field. That is, specific points in depth on the tooth can be observed at higher magnification power with increased resolution, which is very useful when you need fine diagnoses, inspections of structures such as margins, or inside the canal, or when working with ultrasound tips in periodontal microsurgery, endodontic microsurgery, and complex endodontic treatment.13
Recommendations:
- Use low- or medium-magnification steps for active work with manual instruments such as high-speed pieces, sutures, and low-speed pieces.
- Use high-magnification for inspection, detailed diagnosis, or active work in depth at specific points.
Microscopy in fixed prosthodontics
The survival of fixed prosthodontics depends on the state of the marginal adaptation, which is one of the most important technical factors for the long-term success of any restoration. A marginal gap means the entrance of millions of bacteria into the tooth, creating favorable conditions for biofilm deposition, caries, and periodontal disease.14
Several studies of various all-ceramic crown systems have reported a wide range of marginal openings from 0 to 313 μm,15 while others suggest that the use of the microscope with multiple magnification levels increases the possibility of seeing a horizontal marginal gap of 0 μm and vertical marginal fit of 50 μm between the dental prosthesis and abutments affecting the long-term prognosis of the fixed prosthesis.16
In prosthodontics, magnification enhances the surgical field 6x–8x, simplifying the technique and the outcomes,17 also an enhancement related to thickness or roughness on a scale of less than 20 μm.18
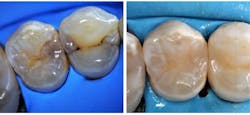
Dental students should be exposed to learning to work with magnifying loupes, as it consistently promotes fewer errors compared to naked eye-dentistry, resulting in better outcomes.19 Laboratory technicians also benefit from high magnification, which improves precision and prosthesis quality, producing marginal discrepancies of < 50 micron. It also allows them to polish the surface of the restorative material with minimal bacterial accumulation (figure 3).20
Clinical aplications:
- Improvement in tooth marginal surfaces detection and preparation.
- Retractor cord placement
- Finest surface matherial polishing
- More precise work by lab technicians
Microscopy in restorative dentistry
Restorative dentistry requires accurate restorations less prone to leakage and decay. Unaided vision has shown decreased outcomes in terms of achieving a tight contact between the filling material and the dentin. High-powered magnification of 4x–6x through magnifying loupes and even greater through a dental microscope increases the visual details from diagnosis to final polishing.21
The dental microscope allows a more conservative cavity preparation, precise placement of restorative materials, and identification of carious lesions and old restorations that need to be replaced.22
Other studies suggest that Magnification improves (figure 4):23
- Cavity detection and removal
- Visibility during direct restorative treatments
- Minimal tooth reduction
- Good finishing of the margins
- Precise sitting of matrices and wedges in proximal cavities treatment
Microscopy in periodontic implants and surgery
The greater magnification provided by a dental microscope following the Cortellini study, improved illumination and view of the surgical field which allowed for proper access to and debridement of the intrabony defect with increased accuracy and minimal trauma.24
One of the greatest advantages of microscope dentistry applied to periodontics, implants, and surgical treatments is the appearance and application of smaller instruments that can be used with high precision due to improved visual acuity.25
Small, sharp tools used in microsurgery enable clean, nonragged incisions which results in improved soft-tissue healing.26
Micro mirrors, elevators, and needle holders smaller than those used in conventional periodontal surgery promote more efficient remotion of tissue pieces, with increased precision and less tissue damage.27
Microsurgical suturing is done with sutures ranging from 6–0 to 9–0 which allows wound closure with sufficient tension and the least possible dead space compared to conventional surgery.
Microsurgical management of soft tissues improves most steps in a procedure; starting with flap design, the precision afforded by increased information from multiple magnification steps and lighting, and the usage of micro instruments promotes faster healing, less traumatic soft-tissue management, and less trauma, and leads to rapid wound-healing and less postop complications.28
The dental microscope in implant dentistry is used in different stages of treatment, from implant placement to peri-implantitis management, allowing for increased precision every step of the way.29
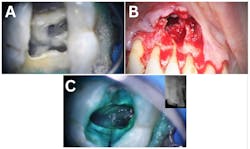
Clinical applications (figure 5):
- Root surface debridement
- Periodontal regeneration
- Mucogingival surgery
- Implant therapy
- Crown lengthening
Microscopy in endodontics
The value of the dental microscope and high magnification in general has been known for many years in this specialty, so much so that in endodontics programs within the US, its usage has been mandatory in university programs since 1998.30 The demands regarding both vision and precision, especially in depth of focus, are more intense in endodontics than in other specialties; in turn, complex, long procedures often require the ergonomic benefits that come with practicing under a microscope.
Working with a dental microscope results in great benefits in performance and quality, accurate diagnosis, endo access, three-dimensional obturation, and final restoration compared to other magnification devices or naked-eye dentistry.31
Benefits include (figure 6):32
- Diagnosis of cracked teeth
- Better visualization of pulp chamber, canal orifices during instrumentation
- Precise identification and removal of obliterations and calcifications
- Precise identification and removal of denticles
- Precise location of hidden canals/canal systems
- Perforation repair
- Removal of fractured posts and instruments
- Surgical endodontics
Conclusion
There is consistent evidence of multiple benefits that come from using dental microscopes for more than just endodontics. All specialties require precise visual information to achieve precise treatment and more predictable results. The idea of seeing better, of seeing magnified in several steps, with light free of shadows, while also promoting better posture and work is more than enough reason for dentists to rely on this technology. Incorporating this technology into dental school will flatten the learning curve. Additionally, following correct usage guides and receiving training based on ergonomic postural laws will result in the fluid use of this tool, which in the next few years should be a standard of teaching and use for all dental professionals of all dental specialties.
Editor's note: This article originally appeared in DE Weekend, the newsletter that will elevate your Sunday mornings with practical and innovative practice management and clinical content from experts across the field. Subscribe here.
References
- Perrin P, Eichenberger M, Neuhaus KW, Lussi A. Visual acuity and magnification devices in dentistry. Swiss Dent J. 2016;126(3):222-235. doi:10.61872/sdj-2016-03-142.
- Tibbetts LS, Shanelec D. Periodontal microsurgery. Dent Clin North Am. 1998;42(2):339-359.
- Vineet RV. Dental operating microscope: the third dimension in dentistry. Adv Dent & Oral Health. 2016;1:555562. doi: 10.19080/ADOH.2016.01.555562
- Liu B, Zhou X, Yue L, et al. Experts consensus on the procedure of dental operative microscope in endodontics and operative dentistry. Int J Oral Sci. 2023;15(1):43. Published 2023 Sep 18. doi:10.1038/s41368-023-00247-y
- Pîrvu C, Pătraşcu I, Pîrvu D, Ionescu C. The dentist's operating posture-ergonomic aspects. J Med Life. 2014;7:177–82.
- Eichenberger M, Biner N, Amato M, Lussi A, Perrin P. Effect of Magnification on the Precision of Tooth Preparation in Dentistry. Oper Dent. 2018;43(5):501-507. doi:10.2341/17-169-C
- Doppalapudi N, Burugapalli RK. Benefits of utilization of magnification in dentistry: a review. Dental Research and Oral Health. 2020;3(3):121-128.
- Tijdschrift voor Ergonomie. Jaargang. 34. nr. 3. June 2009
- Horihata S. Characteristics of light sources for dental instruments. Int J Microdent. 2014;5:72-75
- Perrin P, Neuhaus KW, Eichenberger M, Lussi A. Influence of different loupe systems and their light source on the vision in endodontics. Swiss Dent J. 2019;129(11):922-928. doi:10.61872/sdj-2019-11-565
- Bowers DJ, Glickman GN, Solomon ES, He J. Magnification's effect on endodontic fine motor skills. J Endod. 2010;36(7):1135-1138. doi:10.1016/j.joen.2010.03.003
- Low JF, Dom TNM, Baharin SA. Magnification in endodontics: A review of its application and acceptance among dental practitioners. Eur J Dent. 2018;12(4):610-616. doi:10.4103/ejd.ejd_248_18
- Gogiya RJ, et al. Magnification in dentistry: a review. Int J Appl Dent Sci. 2018;4(2):83-85.
- Zhou Y, Li Y, Ma X, Huang Y, Wang J. Role of span length in the adaptation of implant–supported cobalt chromium frameworks fabricated by three techniques. The journal of advanced prosthodontics. 2017;9(2):124–9.
- Sakrana AA. In vitro evaluation of the marginal and internal discrepancies of different esthetic restorations. J Appl Oral Sci. 2013;21(6):575-580. doi:10.1590/1679-775720130064
- Hirata T, Nakamura T, Wakabayashi K, Yatani H. Study of surface roughness and marginal fit using a newly developed microfinishing bur and a new preparation technique. Int J Microdent. 2009;1:61–64
- van As GA. The use of extreme magnification in fixed prosthodontics. Dent Today. 2003;22:93–99
- Jones CS, Billington RW, Pearson GJ. The in vivo perception of roughness of restorations. Br Dent J. 2004;196(1):42-31. doi:10.1038/sj.bdj.4810881
- Leknius C, Geissberger M. The effect of magnification on the performance of fixed prosthodontic procedures. J Calif Dent Assoc. 1995;23(12):66-70.
- Winter RR, Cornell DF, Vingoren GJ, Patrick RB. Use of magnification in dental technology. J Esthet Restor Dent. 2003;15(7):409-416. doi:10.1111/j.1708-8240.2003.tb00967.x
- Mamoun JS. A rationale for the use of high-powered magnification or microscopes in general dentistry. Gen Dent. 2009;57(1):18-96.
- Moura, JR. Operating microscopes in restorative dentistry: the pursuit of excellence. Int Dent. 2009;10:4-11. Available from: http://www.moderndentistrymedia.com/sept_oct2008/moura.pdf
- Sheets CG. The periodontal-restorative interface: enhancement through magnification. Pract Periodontics Aesthet Dent. 1999;11(8):925-932.
- Cortellini P, Tonetti MS. Minimally invasive surgical technique and enamel matrix derivative in intra-bony defects. I: Clinical outcomes and morbidity. J Clin Periodontol. 2007;34(12):1082-1088. doi:10.1111/j.1600-051X.2007.01144.x
- Yadav VS, Salaria SK, Bhatia A, Yadav R. Periodontal microsurgery: Reaching new heights of precision. J Indian Soc Periodontol. 2018;22(1):5-11. doi:10.4103/jisp.jisp_364_17
- Belcher JM. A perspective on periodontal microsurgery. Int J Periodontics Restorative Dent. 2001;21(2):191-196.
- Belcher JM. Periodontal microsurgery. In: Dibart S, Karima M, editors. Practical Periodontal Plastic Surgery. Oxford, USA: Blackwell Munksgaard; 2006. 15–22.
- Carr GB, Murgel CA. The use of the operating microscope in endodontics. Dent Clin North Am. 2010;54(2):191-214. doi:10.1016/j.cden.2010.01.002
- Duello GV. The use of surgical microscopes in contemporary implant therapy. Pract Proced Aesthet Dent. 2005;17(10):717-718.
- Use of microscopes and other magnification techniques. American Association of Endodontists. 2012. aae.org/specialty/wp-content/uploads/sites/2/2017/06/microscopestatement.pdf
- Kumar et al. Dental Operating Microscope in Endodontics-A ReviewIOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861. Volume 5, Issue 6 (Mar.- Apr. 2013), PP 01-08.
- Alshargawi WK, et al. The impact of dental operating microscopes on the success rates of endodontic treatments. Int J Community Med Public Health.2023;10(8):3000-3003. doi:10.18203/2394-6040.ijcmph20232398
About the Author

Juan Carlos Ortiz Hugues, DDS, CEAS
Juan Carlos Ortiz Hugues, DDS, CEAS, is a master of the Academy of Microscope Enhanced Dentistry (AMED), associate professional in ergonomics by BCPE, CEAS II, and president of the AMED. He wrote the book, Ergonomics Applied to Dental Practice, available from Quintessence Publishing. He provides lectures, training, and advice on advanced dental ergonomics in Latin America and the United States, mainly related to ergonomics applied to dental microscopy.