Reducing or eliminating caries on crown margins
Each month, Dr. Gordon Christensen answers a question from readers about everyday dentistry.
Q: I have been practicing for many years and have placed hundreds of crowns. You have written about why zirconia crowns are frequently coming off, and I have certainly seen that problem in my practice. Now, I am seeing another problem. It is apparent to me that there are more crowns with caries on the margins than I have seen in the past. Why is that happening, and can I stop it?
A: Numerous dental material companies and dental laboratories have been promoting the use of resin cements for zirconia crowns. They state the reason for this is that resin is a strong and relatively insoluble material. Those are great properties. Now, let’s observe other properties of resin cement and laboratory-scanned virtual dies that are not so desirable.
You may remember past questions I have answered in Dental Economics indicating potential reasons why zirconia crowns are coming off more often than crowns cemented with rigid cements, such as zinc phosphate or conventional glass ionomer (GI) cements.1-3 Resin cements are resilient, and zirconia crowns are extremely rigid. Resilient cement appears to be why crowns are coming off. Zinc phosphate and conventional GI cements are rigid and unyielding in the event of an impact on the crown, such as biting with an impact force on any hard piece of food. Rigidity appears to be why the crowns did not come off in service.
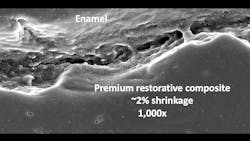
There are some other unfortunate characteristics of resin cement related to your observation of an increase of caries. The resin cements on the current market are composite resins like those being used for tooth restorations but without high filler content. Why is this a problem? Upon polymerization, the resin shrinks, adding another challenge to the already open margins provided by scanning.
Why are scanned margins microscopically open? The margins are open significantly due to laboratory spacing of the virtual dies to allow easy seating. The result of the marginal opening caused by scanning spacing and the polymerization shrinkage creates the possibility for ingress of mouth fluids and food debris (figure 1). All resin-based composite restorations have similar shrinkage and open margins, contributing to the well-known short longevity of these restorations (figure 2).
Reducing caries around crown margins
You cannot avoid open margins on milled zirconia crowns because of the problems described above. What is a potential solution? Use of cariostatic cements to fill the open margins appears to be at least one of the solutions.
During the 1970s and 1980s, conventional GI cement was very popular. However, infrequent and unexpected postoperative tooth sensitivity was a common complaint. Resin-modified glass ionomer (RMGI) soon grew in popularity because, unlike conventional GI, RMGI cements also offer fluoride release and only infrequent postoperative tooth sensitivity.
Is the sensitivity problem still present with conventional GI cements? Yes. If used as in the past, the sensitivity problem would still be present. But over the past several decades, that problem has been solved by using bonding agents and desensitizers containing 5% glutaraldehyde and 35% HEMA (MicroPrime from Zest, Gluma from Kulzer, G5 from Clinicians Choice, and Glu/Sense from Centrix).
The glutaraldehyde coagulates the collagen, closing the dentinal tubules, and the HEMA “wetting” material carries the glutaraldehyde down the dentinal tubules to disinfect the tooth. Although several chemicals can disinfect tooth preps, such as chlorhexidine or benzalkonium chloride, the glutaraldehyde both disinfects and desensitizes.
If cariostatic cements are used, the open margins of current crowns would be much less problematic.
Suggested RMGI and conventional GI cements
Well-known RMGI cements are RelyX Luting Plus from 3M and Fuji Cem Evolve from GC (figure 3). Well-known GI cements are Ketac Cem from 3M and Fuji I from GC (figures 4 and 5).
Technique for using conventional GI cement and desensitizing the tooth
- Place a few drops of glutaraldehyde-containing material in a dappen dish (Gluma, MicroPrime G, Glu/Sense, G5, or others).
- Dip a small microapplicator brush in the liquid (for example, Multi-Brush from Denbur).
- Blot the microapplicator brush, removing most of the liquid.
- Using magnification and adequate light, paint the tooth prep with the glutaraldehyde-containing microapplicator brush, leaving only a damp surface of the liquid.
- Leave the liquid on the prep for one minute.
- Suction off the liquid; do not use air or water during the procedure.
- Repeat the one-minute application of glutaraldehyde procedure.
- Do not get the liquid on the soft tissue to avoid damaging the soft tissue.
- The GI may be hand-mixed to the appropriate viscosity desired or triturator-mixed as developed by the manufacturer.
- Minimally air-dry the tooth.
- Seat the restoration, avoiding contamination.
- Let the material set, remove the debris, and check radiographically for any remaining cement.
Reasons for potential change to conventional GI or RMGI cements (figure 6)
Many research papers support the following statements, so look them up if you have questions.
- The margins of current zirconia crowns are open more than crowns of the past.
- Resin cements have significant shrinkage.
- Resin cement has no cariostatic properties.
- GI chelates to tooth structure without a marginal opening. RMGI chelates also, but it has a slight marginal opening due to its resin component.
- GI has proven high cariostatic properties. RMGI has proven cariogenic properties but less than GI.
- Historical postoperative tooth sensitivity with GI can be overcome with glutaraldehyde-containing solutions. RMGI has only minimal postoperative tooth sensitivity, but glutaraldehyde is still suggested for disinfection.
Technique for using RMGI cement and desensitizing the tooth
Steps 1–8 are the same as for conventional GI listed above.
9. Minimally air-dry the tooth.
10. Seat the restoration, avoiding contamination.
11. Light-cure the RMGI. Most of the current RMGI materials have a light-curing capability for the 20% of the material that is resin.
12. Let the GI part of the material obtain an initial set, remove the debris, and check radiographically for any remaining cement.
Summary
The extremely high use of ceramic crowns is now well-known, with zirconia being the most commonly used. Zirconia crowns are milled producing a potentially esthetic crown but with open margins created by spacing the virtual dies and the milling process. The development of new caries on the margins of these crowns is already appearing. Noncariostatic resin cements are being used by many for zirconia crowns. It is suggested that dentists consider using conventional GI or RMGI cement to reduce caries on the margins of these crowns.
Editor's note: This article appeared in the July/August 2024 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Christensen GJ. Successful cementing of zirconia crowns: Still a problem. Dental Economics. January 5, 2023. https://www.dentaleconomics.com/science-tech/article/14286611/successful-cementing-of-zirconia-crowns-still-a-problem
- Christensen GJ. Solving challenges with zirconia and lithium disilicate crowns. Dental Economics. October 23, 2023. https://www.dentaleconomics.com/science-tech/article/14298889/solving-challenges-with-zirconia-and-lithium-disilicate-crowns
- Christensen GJ. Solving zirconia occlusion challenges. Dental Economics. December 26, 2023. https://www.dentaleconomics.com/science-tech/article/14301401/solving-zirconia-occlusion-challenges
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.