Editor's note: Originally published in 2011. For updated information on CBCT, read CBCT in the dental practice: Creating efficiencies and value.
Technological advances, such as digital imaging systems, have significantly increased the level of detailed information available to practitioners while mitigating the level of patient radiation exposure. While oral health professionals have long relied on 2-D imaging for diagnosis and treatment planning, this technology typically requires multiple exposures, and with them, multiple doses of radiation.
Today, with a properly prescribed 3-D scan, practitioners have gained the ability to collect much more data – often with a single scan and potentially with a lower effective patient dose.
With cone beam computed tomography, oral health professionals gain a highly accurate 3-D image of the patient’s anatomy from a single scan. These 3-D images allow the practitioner to better diagnose and understand the true extent of dental disease, and they can provide for more appropriate treatment for patients.
CBCT should not be used as a substitute for conventional 2-D examinations; rather 3-D should be used as a supplemental exam when it is expected that the 3-D scan will provide additional information, with the potential to enhance the diagnosis or treatment plan.
In recent years, there have been some concerns raised regarding the amount of radiation dosage in medical CT scans. Unfortunately, these reports have created misunderstandings regarding dental scans – specifically CBCT scans.
While radiographs are one of the best diagnostic tools available to medical and dental practitioners, radiation safety has become a critical issue internationally. Repeated patient exposure to radiation over long periods of time is associated with irreversible eye damage, genetic defects, and the development of malignancies in the lens of the eye, thyroid, salivary glands, bone marrow, and skin.
As a result, it is essential that health-care professionals are especially careful and thorough when radiation is used to help ensure minimal exposure to patients. Ionizing radiation should be used only when and where it is indicated.
Patients should always be informed of the potential risks, benefits, and alternatives available to them. Practitioners also should subscribe to the ALARA Principle (As Low As Reasonably Achievable), which dictates that every precaution should be taken to minimize radiation exposure to patients.
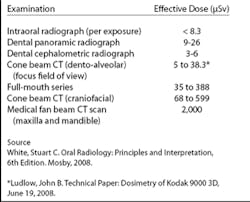
With these reminders of safety of primary concern, the addition of CBCT to an oral health professional’s practice presents with it a significant change in the diagnosis and treatment of dental and maxillofacial areas. The 3-D information obtained from a CBCT exam offers the potential of enhanced diagnosis for a wide range of clinical applications, typically at a lower dose than medical multislice CT (see chart below).
In addition, dental CBCT scans can be collimated to the desired area, further lowering a patient’s exposure to radiation.
Adoption of cone beam computed tomography
Digital imaging has become one of the most important diagnostic tools for oral health professionals, and the greatest advance in the past decade has come with CBCT. It uses a cone-shaped beam and digital processing to reconstruct a virtually distortion-free 3-D image of the patient’s complete skull or dental anatomy in a single pass, depending on the field of view.
This provides dentists and dental specialists with a critical and highly accurate diagnostic and treatment-planning tool. Research has demonstrated the benefits of CBCT over routine dental radiographs in diagnosis of maxillofacial pathosis, bone loss, root resorption, alveolar fractures, implant placement, and more.
The number of practices using CBCT units in Europe and North America is on the rise. In particular, a number of European researchers have explored the risks and benefits of CBCT. They have documented results related to everything from precision in implant placement to long-term radiation doses in pediatric patients. Furthermore, there have been initial proposals for guidelines related to CBCT in Europe.
The European Academy of Dental and Maxillofacial Radiology – a multidisciplinary organization that includes academics and clinicians ranging from dental radiologists to medical physicians – has led the way by introducing a set of standards for CBCT use. This set of 20 "basic principles" offers evidence-based guidelines for dental and maxillofacial use of CBCT.
Certainly, North American researchers and professionals are embracing CBCT as well. Many are working to develop a reference library of data, as well as guidelines related to dosage and professional responsibility. For example, the American Academy of Oral and Maxillofacial Radiology executive committee has begun assembling guidelines and position papers for use of CBCT in endodontics, orthodontics, TMJ imaging, and implant planning.
To be certain, there remain barriers to readily embracing CBCT technology. As with any new diagnostic equipment, many offices may be slow to adopt CBCT systems due to the expense, learning curve, or even regulatory restrictions that vary according to region.
Yet CBCT has become the diagnostic standard, allowing visualizations that simply could not be imagined just a few years ago at doses approximating that of conventional 2-D radiology.
Without evidence-based guidelines on CBCT use, each case requires a specific risk/benefit assessment in comparison to traditional radiographic exams. This assessment also depends on the category of CBCT unit used, considering that not all CBCT units allow practitioners to confine the examination to the region of interest (medium/large field-of-view exams versus focused-field exams). Thus, all CBCT units do not deliver the same dose performance.
To reduce the amount of radiation exposure, dentists should search for a unit that offers control over dose parameters and that can be collimated. Focused field units are a good example since they provide low-dose radiation and a field of view limited to the region of interest.
Patient benefits of CBCT scanning
There are many benefits for patients undergoing a CBCT scan. Compared to regular X-rays, CBCT scans can better differentiate between many types of tissue. This includes bone, teeth, the IAN canal, and limited soft tissue. This increases the likelihood that practitioners will correctly identify pathology.
Because fewer images are needed for diagnosis – often just a single scan will provide accurate diagnostic information – patients are properly diagnosed, triaged, and treated the first time. This reduces treatment ambiguity.
As outlined in the ALARA principle, every precaution should be taken to minimize radiation exposure. Radiation exposure from CBCT is up to 10 times less than that incurred from medical CT scanning, which exposes a patient to a dose of approximately 400 to 1000 µSv.
How does this compare to other forms of radiation, and how do you explain this to patients?
The average effective dose from background radiation is about 3 mSv per year. The adult effective dose from a CT exam of the abdomen is roughly equivalent to the adult effective dose from roughly 400 chest X-rays.
Effective dose of CBCT exams varies depending on the volume of tissues being examined and the anatomical region being examined – the larger the field of view, the higher the radiation dose.
Before performing 3D exams or purchasing a 3-D system, practitioners should select the most suitable volume size considering what clinical applications they expect the system to support. They should follow the guidelines provided by the American Academy of Oral and Maxillofacial Radiology and the European Academy of DentoMaxilloFacial Radiology regarding the limitation of the field of exposure.
Large FOV is ideal for maxillofacial surgery or as a diagnostic tool for patients with facial trauma, while medium FOV is well-suited for implantology that involves multiple quadrant and TMJ examinations. Focused FOV is primarily for dento-alveolar applications. This includes endodontics, single quadrant implant cases, and local dental problems.
CBCT units delivering the lowest doses are nearly equivalent to the dose of the panoramic exam, allowing dental professionals to benefit from the power of 3-D while limiting the risk associated with radiation exposure.
In addition, CBCT systems using a smaller FOV have a higher image resolution in addition to lower doses. This increases the applications of CBCT to include endodontics, oral surgery, and orthodontics, especially with units that combine 3-D imaging with panoramic/cephalometric imaging.
Diagnostic benefits of CBCT/3-D imaging
CBCT is useful in a variety of diagnostic situations, including but not limited to oral surgeries, implant planning, TMJ analyses, airway studies related to sleep apnea, impacted teeth, periodontal diseases, and endodontic anomalies. The high-resolution 3-D images allow practitioners to more accurately visualize internal anatomy, assess risk, and plan treatment and surgery.
The scans can be used to assess bone quality, which is essential to evaluate if there is a sufficient amount of bone for implant placement, and utilized to quickly identify the size and location of a lesion. CBCT can also be helpful in orthodontic analysis, including the detection and localization of airway problems and skeletal asymmetries.
By comparison, 2-D images show only the length and breadth of the anatomy with distortion. CBCT adds depth, thus giving the clinician multiplanar views of the volume. This further improves diagnostic abilities and reduces the need to take multiple X-rays.
The 360° model of the patient that results from the CBCT scan can be rotated, and slices can be isolated and manipulated for analysis. CBCT imaging offers a tremendous advantage compared to 2-D radiographs since practitioners must compensate for superimposition and distortion often present in 2-D radiographs.
Hybrid units that include both 2-D and 3-D imaging allow dental professionals a way to optimize the dose in a manner that is not possible with large- and medium-field systems that lack 2-D modality. Further, like 2-D radiographs, 3-D scans may be easily shared among practitioners.
For example, an implant planning site can be chosen, virtual implant placed, and data shared with the restorative dentist to rule out any potential issues when placing the implant. Not only does this ensure that all clinicians involved in a patient’s care are working from the same data, it also elevates the standard of care and satisfaction by reducing the need for the patient to undergo multiple scans for each practitioner.
Conclusion
One of the most important dental diagnostic innovations has been the advent of cone beam computed tomography, which has proven effective for many applications in oral health care. CBCT is a technology that is considered by some to be the standard of care where 3-D imaging is necessary in dentistry. This technological leap allows practitioners to gain immediate access to accurate 3-D images of anatomical structures, which often are critical to precise diagnoses, more effective treatment planning, and increased case acceptance.
As CBCT is adopted by more practitioners, it will continue to provide numerous benefits for practitioners and patients alike. This should include improved outcomes, reduced need for exploratory procedures, improved treatment predictability, reduced morbidity, and potentially lowered cost and time savings.
Ken Serota, DDS, MMSc, is an author of more than 70 publications. He has lectured on endodontics and implantology around the world. He received his MMSc from the Harvard-Forsyth Dental Center in Boston, Mass., and is a Fellow of the Pierre Fauchard Academy. Dr. Serota is the founder of ROOTS, a global online educational forum for dentists who wish to learn cutting-edge endodontic therapy.