How does glutaraldehyde prevent postoperative tooth sensitivity?
Dr. Gordon Christensen discusses one of the simplest and most foolproof procedures to prevent postoperative tooth sensitivity and disinfect tooth preparations—the use of glutaraldehyde-containing desensitizing/disinfecting solutions.
Q:
I have tried numerous methods to desensitize tooth preparations, but I still experience postoperative tooth sensitivity occasionally with both direct and indirect restorations. I am frustrated by this challenge because patients often think that the sensitivity is my fault. What can be done to reduce or eliminate this problem?
A:
It is interesting to note that some dentists have patients who complain of postoperative tooth sensitivity frequently, while others do not. The question you asked is not a new one; it has been asked for several decades. Scientists and clinicians in our research organization, Clinicians Report Foundation (CR Foundation), have researched this topic for many years.
Numerous materials and clinical techniques have been described to prevent postoperative tooth sensitivity, and some are quite effective. However, only a few techniques both desensitize and disinfect tooth preparations.
The techniques vary:
• Specific procedures for placing typical bonding agents
• Use of liners
• Use of solutions such as chlorhexidine, benzalkonium chloride, sodium hypochlorite, or glutaraldehyde on the tooth preparations
• A combination of the above chemicals
• Many other concepts
You asked about glutaraldehyde, and I will limit this discussion to that topic only. This chemical has been used in dentistry successfully for decades for instrument disinfection and various treatments for tooth preparations. What does glutaraldehyde do to tooth structure? Research shows that adequate use of glutaraldehyde on tooth structure for a prescribed period of time successfully disinfects the tooth. Additionally, glutaraldehyde coagulates collagen, a major component of dentin. As it coagulates the collagen, microscopic research shows that the thousands of dentinal canals in the tooth are closed, thus reducing the ability of the dentin to transmit pain stimuli to the pulp.1 When glutaraldehyde is placed on tooth preparations, the teeth are not sensitive postoperatively.
This is not new research. It has been known for several decades. The TRAC Division of the CR Foundation, directed by Dr. Rella Christensen, has spent years researching this topic. (This research is available by searching cliniciansreport.org.). However, in spite of positive research on the use of glutaraldehyde for tooth disinfection and desensitization, it is still controversial among some clinicians and researchers.
The following information is intended to provide support for the use of glutaraldehyde-containing solutions for both tooth desensitization and disinfection.
Example brands of glutaraldehyde-containing solutions
The original, well-proven, long-used glutaraldehyde solution is Gluma Desensitizer (Heraeus Kulzer). Other competitive brands are G5 All-Purpose Desensitizer (Clinician's Choice Dental Products Inc.), Glu/Sense (Centrix Inc.), MicroPrime (Danville Materials), and Telio CS Desensitizer (Ivoclar Vivadent). These solutions contain 5% glutaraldehyde and 35% hydroxyethylmethacrylate (HEMA).
Soft-tissue irritation
There is no question that indiscriminate, sloppy use of glutaraldehyde solutions can irritate soft tissue, creating lesions that simulate aphthous ulcers, especially in the mucobuccal fold where excess solution can collect. This criticism is valid, and care must be exercised to prevent this challenge.
The following technique reduces this problem:
1. Use a small microbrush (commonly used for placing bonding agents) to place the glutaraldehyde solution on the tooth.
2. Place the microbrush into a small amount of glutaraldehyde solution in a dappen dish or a single-use product. Make sure the microbrush is not too wet.
3. Blot the microbrush on a piece of paper. It should be damp only.
4. Place the microbrush tip into the direct tooth preparation or onto the indirect tooth preparation. The liquid will flow slowly since it contains the wetting agent (HEMA) that stimulates its wetting of the tooth preparation.
How long should the glutaraldehyde solution be left on the tooth?
Microbiologic research has shown that for optimum disinfection, the solution should be left in contact with the tooth structure for two one-minute applications. This may seem like a long time, but the microbiology research shows that it is necessary for optimum disinfection.
Should the glutaraldehyde solution be washed off?
There is some controversy on this topic in the literature, and also in the instructions of companies based on whether or not they produce glutaraldehyde solutions. The reasons for the controversy are varied.
Some say glutaraldehyde should not be used on tooth preparations because it reduces the effectiveness of the bond to be subsequently placed. Research at CR Foundation has disproven that allegation. The bond of popular bonding agents is slightly improved by using glutaraldehyde solutions.
Some say to blow the residue off of the solution. This is not appropriate, because the excess liquid remaining on the tooth preparation can be blown onto the soft tissue, injuring it and causing later discomfort.
Some say to wash off the glutaraldehyde. The solution has been placed to desensitize the tooth by stimulating the entry of the glutaraldehyde into the dentinal canals. HEMA does just that. Washing off the solution defeats much of the effect of using the solution.
The proper technique after placing the glutaraldehyde for two one-minute applications is to place a high-velocity suction tip directly over the tooth, turn it on, and let the suction evacuate any excess material left on the tooth. Use of a very light air stream to blow the excess into the suction device is advocated if suction is not adequate.
In which clinical situations should glutaraldehyde be used?
Glutaraldehyde should be used in any situation in which you want to desensitize and disinfect tooth preparations-from sealants through all classifications of restorations, to tooth preparations for full-mouth rehabilitations.
Are there any negative effects related to glutaraldehyde use?
In spite of allegations about the negative effects of glutaraldehyde use from various sources, the reverse has been evident. Many clinicians who have patients suffering from lingering tooth sensitivity have asked how to reduce or eliminate postoperative sensitivity. When clinicians follow our advice regarding how to use the solutions, we have received very positive comments about prevention of postoperative tooth sensitivity. Of course, care must be taken to avoid harm to the soft tissue.
In what sequence should the solutions be used?
When placing resin-based composite, the solution should be placed directly after the tooth preparation is completed-before any base, liner, or bonding agent is placed. When placing glutaraldehyde on a crown preparation, it is suggested that the solution be placed immediately before cementing the indirect restoration. Some clinicians report the desirability of also placing glutaraldehyde at the time of finishing the indirect tooth prep before cementing the provisional tooth restoration. Use of either or both techniques has shown clinical success.
What is a typical procedure for use of glutaraldehyde for a Class II restoration?
The following procedure is suggested for use of glutaraldehyde for Class II resin-based composite restorations (figures 1-6).
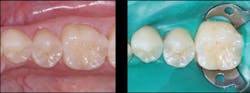
Figure 1: Apparently small caries on distal of mandibular second premolar
Figure 2: Tooth isolated and ready for tooth preparation with No. 329 bur on mandibular second premolar
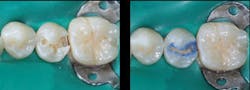
Figure 3: Tooth preparation initially cut (left) and cut deeper (right) showing inadequacy of current generation of digital bitewings to show full extent of caries as related to radiograph
Figure 4: Final prep (left) and acid placed for selective etch of enamel only (right). Liner was not placed in this prep. Etch-and-rinse (total-etch), selective, and self-etch techniques have been shown to be adequate.
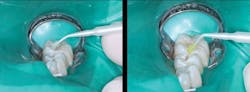
Figure 5: Glutaraldehyde placed for two one-minute applications and suctioned off (left) followed by your choice of bonding agent (right)
Figure 6: Finished restoration. Restorations accomplished in this manner will not have postoperative tooth sensitivity.
When using the etch-and-rinse (total-etch) method, or the selective etch of enamel only, the following technique is suggested:
1. Prep.
2. Place glutaraldehyde for two one-minute applications and carefully suction off the excess.
3. Place a liner in deep areas if needed.
4. Etch either the complete prep or only the enamel.
5. Wash and dry the prep, noting that you have also washed off the solution.
6. Again, place glutaraldehyde for one short application, since the previous application has been washed off areas of the tooth not covered with base.
7. Place the bonding agent.
8. Place the resin.
When using the self-etch bonding method, the following technique is suggested:
1. Prep.
2. Place glutaraldehyde for two one-minute applications and carefully suction off the excess.
3. Place a liner in deep areas if needed.
4. Place the bonding agent.
5. Place the resin.
Summary
Numerous methods are claimed to reduce or potentially prevent postoperative tooth sensitivity in teeth receiving resin-based composite restorations, crowns, and fixed prostheses. One of the simplest and most foolproof procedures to prevent postoperative tooth sensitivity and disinfect tooth preparations is the use of glutaraldehyde-containing desensitizing/disinfecting solutions. Follow the detailed technique explained in this article.
Reference
1. Disinfection of Tooth Preparations—Why and How? Clinicians Report. 2009;2(11).
Gordon J. Christensen, DDS, MSD, PhD, is a practicing prosthodontist in Provo, Utah. He is the founder and CEO of Practical Clinical Courses, an international continuing-education organization initiated in 1981 for dental professionals. Dr. Christensen is cofounder (with his wife, Dr. Rella Christensen) and CEO of Clinicians Report (formerly Clinical Research Associates).
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.