by Richard H. Nagelberg, DDS, and Kimberly Miller, RDH, BSDH, RDHMP
For more on this topic, go to www.dentaleconomics.com and search using the following key words: diabetes, oral-systemic link, periodontitis, Dr. Richard Nagelberg, Kimberly Miller.
Ongoing global research continues to address the oral-systemic connections and their impact on total health and wellness. The consensus in the medical and dental professions is that there is an association between the mouth and the body; however, the strength of the association will be unraveled by further research, in particular, interventional studies in which periodontal treatment is provided and the effects on systemic events are observed.
Among the various systemic links to gum disease, the strongest is the connection to diabetes. Diabetes is a group of chronic diseases characterized by hyperglycemia (high blood sugar levels) resulting from defects in insulin production, action, or both. It is estimated that diabetes affects approximately 23.6 million people of all ages in the United States. The National Institute of Diabetes 2007 statistics also estimate that about 5.7 million of these people are undiagnosed diabetics.
These individuals are totally unaware they are diabetic. This report goes on to say that about 2.6% of those aged 20 to 30 have diabetes, while 10.8% of those aged 40 to 59 have diabetes. It was staggering to discover that of those aged 60 and above, 23.8% have diabetes. In other words, one out of every 4.2 patients you see in your dental office over the age of 60 will likely have diabetes.
The mechanism of diabetes
To better understand the mechanism of diabetes, it's important to know the primary players, which are carbohydrates and insulin. Insulin is a protein hormone that gets its name from the Latin insula for island, which is appropriate since it is produced by the beta cells in the islets of Langerhans in the pancreas. Insulin is an essential element in the control of intermediary metabolism, which is the process within cells that extracts energy from nutrient molecules and uses that energy to construct cellular components.
Ingested carbohydrates are broken down in the small intestine into glucose, which is then absorbed into the bloodstream. The elevated glucose in the blood stimulates the release of insulin from the pancreas into the bloodstream. Insulin facilitates the uptake and utilization of glucose in muscle and fat cells throughout the body. All tissues in the body do not require insulin for glucose uptake, including the brain and the liver. These tissue types use another, noninsulin-dependent glucose transporter.
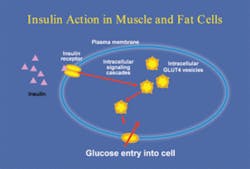
There is a receptor for insulin embedded in the cell membrane of the target cells. Insulin binding to the receptor causes activation of the receptor, which then sets off a series of events inside the cell, rapidly culminating in the movement of internal compartments, or vesicles, inside the cell, to another part of the cell membrane. The vesicles contain the glucose transporters, which then provide an opening in the cell membrane for the uptake of glucose from the bloodstream into the interior of the cells (Fig. 1).
Insulin also stimulates the liver to store glucose in the form of glycogen and is involved in the importing of proteins into the cells. Any disease or condition that interferes with the movement of glucose into the cells leads to hyperglycemia.
Type I diabetes
Type I diabetes, formerly called juvenile diabetes, is most commonly diagnosed in children and young adults and accounts for 5% to 10% of all diagnosed cases of diabetes. It is characterized by the failure of the pancreas to make insulin. This malfunction is usually caused by autoimmune destruction of the pancreatic beta cells. People with type I diabetes need several insulin injections per day or an insulin pump to survive. Most people with type I diabetes eventually develop one or more complications, including damage to the eyes, nerves, kidneys, and blood vessels. Type I diabetics are about 10 times more likely to have heart disease than nondiabetics.
Type II diabetes
Type II diabetes is the most common form of diabetes and accounts for 90% to 95% of all diagnosed cases. Type II diabetes, formerly called adult onset diabetes, is characterized by insulin resistance in the target cells. In other words, the fat and muscle cells do not use insulin properly. Type II diabetes is treated with a combination of dietary modifications, oral medications, and insulin injections if necessary.
Another staggering statistic reported by a recent study suggests that 82% of diabetic patients with severe periodontitis experienced the onset of one or more major cardiovascular, cerebrovascular, or peripheral vascular events compared to only 21% of diabetics without periodontitis.
Take just a moment to reflect upon how many patients you see with diabetes and their periodontal condition; you, too, will feel the magnitude of these statistics. We have an incredible opportunity as clinicians to assist our diabetic patients with their overall health by treating periodontal disease early and assertively.
Complications of diabetes
The importance of preventing hyperglycemia cannot be overstated. Elevated blood sugar in the vascular system is the major source of complications in type I and type II diabetes. Diabetic complications include retinopathy, nephropathy, neuropathy, and cardiovascular diseases. These complications are dramatic and potentially life changing.
Diabetic retinopathy is responsible for approximately 10,000 new cases of blindness in the United States each year. Diabetic nephropathy is the leading cause of kidney failure in the United States, while more than 80% of foot amputations are the result of injury from diabetic neuropathy. Furthermore, cardiovascular disease is the leading cause of death for patients with type I or type II diabetes.
Periodontal disease and diabetes
Diabetic individuals are predisposed to periodontal disease through several mechanisms. Poorly controlled diabetics have diminished salivary flow, leading to xerostomia. The body's ability to kill oral bacteria is considerably diminished as well. Hyperglycemia significantly diminishes the ability of white blood cells, neutrophils in particular, to track, adhere to, and kill bacteria. Additionally, elevated blood sugar leads to elevated glucose levels in the gingival crevicular fluid (GCF). Elevated GCF glucose levels hinder the wound healing capacity of fibroblasts.
Evidence also indicates that periodontal disease can worsen glycemic control. It is well established that infectious and inflammatory processes increase insulin resistance, leading to hyperglycemia. Periodontal disease has both infectious and inflammatory components.
If research demonstrates that periodontal treatment has a beneficial effect on diabetic control, it would provide evidence for the impact oral health has on general health. Two studies demonstrated significant improvement in blood sugar levels after nonsurgical perio treatment. In these studies, nonsurgical treatment was provided on diabetic and nondiabetic perio patients. Both groups of patients showed improvement in their periodontal condition.
The diabetic study subjects showed improved blood sugar control three and six months after periodontal treatment. This information should be highly motivating for dental professionals to continue to assertively recommend treatment to all periodontal patients with diabetes.
It is interesting to note that there are only small differences in the subgingival microbiota between diabetic and nondiabetic periodontal patients, which suggests that the body's immuno-inflammatory response plays the major role in the increased incidence and severity of gum disease commonly seen in poorly controlled diabetic individuals.
The dental professional's role
It is clear at this point that maintaining good oral health and controlling existing periodontal diseases has implications far beyond the oral cavity. Optimal oral health is only possible if dental providers and patients do their respective parts.
Here are a few suggestions to improve your clinical protocols involving the treatment of diabetic patients:
• Ask all patients with diabetes for the results of their last HbA1c test and consider the HbA1c score when treatment planning. This blood test measures the percent of glucose attached to red blood cells. The test gives an accurate indication of how well diabetes has been managed over the preceding two to three months. The HbA1c level is the primary parameter physicians use to monitor blood sugar control for their diabetic patients. Well-controlled diabetics have an HbA1c of 5% to 7%. Readings of 8% and above indicate poor glycemic control. Well-controlled diabetics have the same risk of developing periodontal disease as nondiabetic individuals. Poorly controlled diabetics have a much greater risk of several complications, including periodontal disease. Periodontal treatment outcomes for well-controlled diabetic patients will be the same as nondiabetics. Poor glycemic control contributes to less predictable treatment results, and may factor into the type of periodontal therapy undertaken.
• Visit www.perioeducation.com and click on the Research Plus link to access the “Defeat Diabetes Screening Test” from PerioFrogz.
• Use the Diabetes Screening Test for:
→ Every new patient with a family history of diabetes
→ Annually for all patients over the age of 60
→ All existing patients during health history and risk assessment updates and thereafter every five years unless over the age of 60
• Obtain a color copy of the HbA1c graph for use as a visual aid in each operatory. Print your copy by downloading from www.perioeducation.com. Click on the Research Plus link to access the HbA1c graph from PerioFrogz. Once you have printed the graph, laminate it and keep one in each operatory.
With the current understanding of the relationship between periodontal diseases and overall health and wellness, as dental professionals we are obligated to educate our diabetic patients on the importance of good oral health.
It is no longer optional for us to provide in-depth risk assessment, including questions about diabetes. According to the AAP, “Risk assessment goes beyond the identification of the existence of disease and its severity, and considers factors that may influence future progression of disease. Identifying adverse changes in risk factors, which might be suggestive of disease onset or progression, is an important clinical concept.”
As ongoing research continues to address the oral-systemic connections and their impact on total health and wellness, the consensus in the medical and dental professions is that there is an association. And in our opinion, this association should be addressed with every patient who could be impacted by this information.
While interventional studies and ongoing research continue to expand knowledge, we can do our part daily now, for all patients every time they are under our care, to thoroughly assess their level of risk and fulfill our obligation to provide comprehensive treatment recommendations.
References available upon request.
Meet the PerioFrogz: Richard Nagelberg, DDS, and Kim Miller, RDH. Visit them at perioeducation.com. Richard H. Nagelberg, DDS, has been practicing general dentistry in suburban Philadelphia for more than 26 years. Kimberly Miller, RDH, BSDH, RDHMP, is a partner of the JP Institute and a cofounder of PerioFrogz. As a graduate from Loma Linda University in 1981, she received a bachelor's degree in dental hygiene.