The study of breathing and sleep disorders has been the hottest topic in dentistry over the last couple of years. Patients reporting symptoms—including sore masticatory muscles and temporomandibular joints (TMJs), bruxism, headaches, fatigue, and dental malocclusions—often demonstrate signs of airway and breathing dysfunction. This may involve allergies, upper airway resistance (UAR), mouth breathing, tongue-tie and thrusting, swallowing disorders, and breathing disordered sleep, including obstructive sleep apnea (OSA).
The discipline of Integrative Dental Medicine (IDM) expands Dr. Peter Dawson’s original Concepts of Complete Dentistry model by addressing systemic issues such as airway, breathing, and sleep dysfunction in evaluating dental malocclusions. As such, our eyes have been opened to a new understanding, guiding us to a key principle: dysfunctional breathing can trigger significant oral dysfunction and dental malocclusions. Our enthusiasm for the role of airway dysfunction must be tempered by a word of caution, however: don’t throw the baby out with the bathwater! The critical concept of the importance of TMJ health and integrity in diagnosing masticatory system disorders is just as important as ever, providing another key principle: joint deformation can trigger significant oral dysfunction and dental malocclusions.
The following clinical case study will demonstrate both of these important principles. A 42-year-old female presents for evaluation of progressive facial and dental occlusion changes (figure 1).
Developed by DeWitt Wilkerson, DMD. Copyright 2018 The Dawson Academy. Used with permission.
Each category is then studied in three ways:
• History: Signs and symptoms
• Evaluation: Clinical signs
• Screening and testing, as needed
Utilizing the checklist for our case study, red flags are identified as listed under each of the three categories.
History: Signs and symptoms
Infection/inflammation: Negative—caries, toothaches, bleeding gums, oral sores, tobacco, toxins, high blood pressure, pro-inflammatory diet, chronic pain or stress, diabetes, gastric reflux, physical inactivity
Airway/breathing disorders:Positive—mouth breathing, snoring, poor sleep quality, nasal congestion with allergies, forward head posture, deviated septum; Negative—snoring, sleep apnea, daytime sleepiness, tongue-tie, chronic cough
TMD/occlusion disorders:Positive—joint discomfort, popping/clicking, sore muscles, bruxism, worn teeth, tongue thrust, crooked teeth; Negative—nerve pain, limited opening
Evaluation: Clinical signs
Infection/inflammation:Negative—visual inspection, periodontal probing, oral lesions, lymph nodes, swollen tonsils
Airway/breathing disorders:Positive—Mallampati score >2, scalloped tongue, nasal stenosis, skeletal profile; Negative—neck circumference >16”, 40% tongue restriction
TMD/occlusion disorders: Positive—CR to MIP slide; Negative—ROM atypical, muscle palpation, joint palpation, TMJ load testing
Screening and testing
Infection/inflammation:Negative—radiographic imaging (abscessed teeth), oral cancer screening
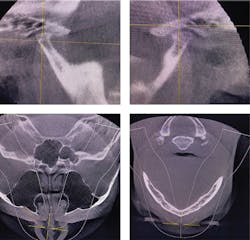
Airway/breathing disorders:Positive—imaging (CBCT deviated septum, narrow posterior airway; figure 3); Negative—overnight pulse oximetry
TMD/occlusion disorders:Positive—Doppler auscultation (joint crepitus), imaging severe joint degeneration (figure 3)
Differential conclusion
Infection/inflammation:Negative
Airway/breathing disorders: Positive for upper airway resistance syndrome (UARS); bimaxillary retrusion with posterior airway obstruction
TMD/occlusion disorders:Positive for severe degenerative joint disease (DJD); severe anterior open-bite malocclusion
Key principles reflected
In this case study, the dental malocclusion reflects the two key principles. Dysfunctional breathing can trigger significant oral dysfunction and dental malocclusion changes. It appears that airway dysfunction in the form of UARS has been caused by allergy congestion and a deviated septum. This could have led to mouth breathing, tongue reposturing and thrusting, forward head posture, bimaxillary retrusion, and bite changes, but that is not the whole story of this case.
Joint deformation can trigger significant oral dysfunction and dental malocclusion changes. The patient was not aware of a specific history of injury initiating bilateral changes in the temporomandibular joints. She did recall a period of time in her 20s when joint clicking was present, but without pain. She has a history of chronic clenching and grinding.