We’ve all had restorative appointments where we’ve removed caries, and the pulp chamber begins to taunt us with its proximity to our bur. Or, we actually have a pinpoint exposure and then try to convince ourselves that the red we’re seeing is really from the bleeding gums and not the nerve of the tooth. Ah, yes, a day in the life of a general dentist. These are the kinds of occurrences that can make restorative appointments and the potential follow-up visits from the patient . . . interesting.
When these situations happen, what’s your protocol? Fill it? Line it? Base it up? It’s routinely taught in dental schools1,2 that in these instances, putting some kind of barrier to protect the tooth or initiate repair is the standard of care. Bases, liners, and cements are the go-to, but which one is best for what scenario? Does it really matter? Some argue that as long as you place something on the cavity floor that acts as a “buffer” between the filling and pulp, you’re golden. But recent research has called into question the clinical protocols and application of these materials, creating a conundrum for practitioners as to what is truly beneficial and necessary.
What do bases and liners really refer to?
In the literature, the terms liners and bases/cements are often used synonymously and interchangeably, which can lead to some confusion as to what each material is and where it can best be applied in a clinical setting. To clarify, we will reference these definitions:
Liners refer to a thin layer of material
(0.5 mm) placed on the surface of the tooth preparation that, in part, protects the tooth from the restorative material (residual reactants diffusing out of the restoration), intraoral fluids, initial electrical insulation, some thermal insulation and, ultimately, from the outside environment; liners usually do not have sufficient thickness, hardness, or strength to be used alone in a deep cavity.1-3
Bases/cement bases (play a two-role definition) are typically a thicker placement of material (1–2 mm) and are used to provide thermal and chemical protection for the pulp and to supplement mechanical support for the restoration by distributing local stresses from the restoration across the underlying dentin surface.2,3
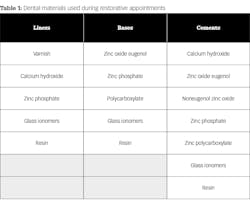
Table 1 provides a general reference to materials that are used in the clinical setting.4 As you can see, several materials are interchangeable in their application by definition. Furthermore, “various liners and bases may be combined in a single preparation, and the total cavity preparation base may be described as the combination of natural dentin, liner, and base.”3
To understand the actions of these agents and how they work, we refer to our basic tooth anatomy. Dentinal tubules contain outward cellular extensions of the pulpal cells and are surrounded by dentinal fluid.3 In the event that there is an insult to the dentin, sensitivity occurs when the mechanoreceptors within the pulp sense the pressure change that occurs when the fluid flows in and out of the tubules. The deeper the caries excavation, the greater the insult to the tooth, and the more the need to consider and manage protection to these five issues increases: (1) chemical, (2) electrical, (3) thermal, (4) pulpal, and (5) mechanical.
Traditionally, dental schools have taught that caries removal was always followed by the placement of a liner, typically a glass ionomer or calcium hydroxide. However, as amalgam has been phased out as a restorative material of choice and resin composites have moved in, questions have arisen as to the validity of this practice.5
An interesting study by Blum et al. recently concluded that “the use of linings beneath posterior composites in clinical practice was not evidence based, with a strong indication that the management of operatively exposed dentin in moderately deep cavities is a vexed issue amongst practitioners.”5 Despite this finding, “the placement of linings under posterior composites remains popular among dental practitioners . . . ignoring the studies that showed that the dentin-sealing effect of bonding agents provides adequate protection and renders the dentin insensitive.”5 Additional research theorizes that “postoperative sensitivity is not caused by the restoration but by bacteria and their byproducts.”2
The question then becomes: do we line or base our preparations prior to restoration placement? The answer, at best, is definitely not black-and-white, as one could make a strong case in either direction. So keep the following in mind:
• Recent research indicates that the need for bases and liners is not as important as it once was due to a shift in how teeth are restored (i.e., amalgam versus composites).
• Continued advancements in bonding agents and their application has and will continue to improve, therefore having an impact on the sensitivity of teeth.
• The quality of resin composites—from the fillers used to the esthetic components and their overall ability to function in a comprehensive manner—is continuously evolving. Furthermore, resin composites themselves can act as a liner.
• The placement of these materials should be considered on a case-by-case, tooth-by-tooth basis as conditions vary.
• Isolation and the use of etches with various cements, bonding agents, and techniques will also have a role in the level of sensitivity.
With that said, validation of your call as to what, when, and where you use bases/liners and cements can be justified with knowledge of the characteristics and functionality of the materials. Keep in mind that if one were to play devil’s advocate, research (under certain circumstances) may contradict what you’ve been doing all along. There is not a one-size-fits-all scenario in medicine, and dentistry is definitely not an exception. The following is a brief summary of the four most common bases and liners.
Glass ionomers—(gi)
• Release fluoride ions
• When placed over decalcified dentin in close proximity to the pulp, they can promote remineralization, even in areas of active caries6
• Use of GIs tends to reduce the probability of marginal gap formation, especially at the gingival margins1,6
• When used as a cement, due to hygroscopic expansion, seal and bond strength of GIs can be significant6
• Product examples: Vitrebond (3M ESPE), Fuji Lining LC (GC America), Ketac Bond and Ketac Cem (3M ESPE), GlasIonomer Base Cement (Shofu Dental Corporation)
Calcium hydroxide—ca(oh)2
• Suspended in a solvent that, when evaporated, leaves behind a layer of Ca(OH)2
• Has a history of high popularity among general dentists as the liner of choice in deeper cavities1
• The high pH (9–12) creates a cytotoxic effect that instigates the formation of a dentinal bridge, which is beneficial on carious dentin and exposed pulp.
• The drawback: it’s soluble, doesn’t bond to dentin, and microleakage can occur over time, which subsequently, to some degree, can leave a restoration unsupported and lead to fracture/failure4,5
• Easy manipulation, rapid hardening, a good seal if completely under a restoration7
• Product examples: Dycal (Dentsply Calk), Life (Kerr Dental)
Zinc oxide eugenol
• Neutral pH and considered the least irritating of all dental materials7
• Provides excellent seal at the restoration-tooth interface, despite the fact that it does not adhere to tooth structure7
• Can be prepared as a thick or thin material and is commonly used as a lower-strength base7
• Product examples: IRM (Dentsply Caulk), Temp-Bond (Kerr Dental)
Resins
• Bonded to tooth structure with adhesives
• Can be technique sensitive depending on the application (etch, self-etch, etc.)
• Polymerization shrinkage can be high with the risk of bond disruption. This results inpoor sealing of the dentin, causing a buildup of bacterial by-products, irritation to the pulp, sensitivity, and potential carious changes of the dentin substrate.5
• Various forms: filled/unfilled, flowable, bases, and cements
• Product examples: AdheSE (Ivoclar Vivadent), Clearfil products (Kuraray Noritake Dental), Tetric Flow (Ivoclar Vivadent), Virtuoso Flowable (DenMat), Venus (Kulzer), Encore (Centrix),
LuxaCore (DMG America), TempBond Clear (Kerr Dental), RelyX Unicem (3M ESPE), G-CEM Resin Adhesive Cement (GC America)
There you have it—the not-so-black-and-white 101 on bases and liners. The initial need and genesis for these materials was, and still is, simple: to provide protection to the pulp, eliminate postoperative sensitivity, and maximize the tooth’s ability to recover. Recent advances in materials, an increased understanding of their application, and the perpetual evolution of dentistry stress the need for us to constantly evaluate how we perform as practitioners, hence the importance of continuing education and communication among colleagues.
References
1. Arandi NZ. Calcium hydroxide liners: a literature review. Clin Cosmet Investig Dent. 2017;9:67-72. doi:10.2147/CCIDE.S141381.
2. Weiner R. Liners, bases, and cements: an in-depth review, Part 1. Dent Today. 2008;27(5):72, 74, 76; quiz 78.
3. Sturdevant CM, Roberson TM, Heymann HO, Sturdevant JR. Bases dental materials. In: Sturdevant CM, Roberson TM, Heymann HO, Sturdevant JR, eds. The Art and Science of Operative Dentistry. 3rd ed. St. Louis, MO: Mosby; 1994:235-239.
4. Weiner R. Liners, bases, and cements: material selection and clinical applications. Dent Today. 2005;24(6):64, 66-72; quiz 73. http://www.dentistrytoday.com/ce-articles/364-liners-bases-and-cements-material-selection-and-clinical-applications. Published June 1, 2005. Accessed September 4, 2018.
5. Blum IR, Wilson NHF. An end to linings under posterior composites? J Am Dent Assoc. 2018;149(3):209-213. doi:10.1016/j.adaj.2017.09.053.
6. Weiner R. Liners, bases, and cements: an in-depth review, Part 3. Dent Today. 2008;27(11):65-66, 68, 70; quiz 71, 64.
7. Weiner R. Liners, bases, and cements: an in-depth review, Part 2. Dent Today. 2008;27(8):48, 50, 52 passim; quiz 55.