Reducing recurrent caries in composite restorations
Each month, Dr. Gordon Christensen answers a question from readers about everyday dentistry.
Q: I have been placing and observing composite resin restorations for many years. During that time, I have also continued to place and observe amalgam restorations. There is no question that I see far more recurrent caries around composite restorations than amalgam restorations. Patients like tooth-colored restorations, and I continue to use them. But redoing the composite restorations as they get new caries cuts away more tooth structure, costs patients more money, and eventually many of the teeth end up needing crowns. What can I do to reduce the obvious problem of recurrent caries around composite restorations?
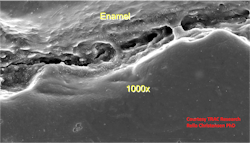
A: Your question is a common one I receive during my continuing education courses, and most dentists would agree with you. Composite restorations look good for a few years, and then caries begins again (figure 1). I shouldn’t say caries begins again. It would be better to say the organisms causing caries in the original lesion had penetrated down the dentinal tubules, and your composite restorations only put a plug in the tooth prep, leaving the organisms to continue their activity.
Rather than the term “recurrent caries,” a more logical one is “continuing caries.” Most dentists are not disinfecting tooth preparations. Instead, they are only placing a plug in the infected tooth preparation and letting the lesions continue to progress. As far back in dental history as Dr. W. D. Miller, an oral microbiologist in the late 1800s, and the well-known Dr. G. V. Black in the early 1900s, many statements were made by both suggesting the microorganisms in caries must be disinfected to stop the caries process. Let’s start the answer to your question with that concept.
Disinfect the tooth prep
Many disinfectants have been used to kill organisms in or on tooth preparations. A few well-known ones are benzalkonium chloride, chlorhexidine, ethanol, isopropanol, peracetic acid, eugenol, and others. They disinfect to various levels of effectiveness, but most do not desensitize the tooth. Glutaraldehyde disinfects and desensitizes teeth when combined with ethylenediaminetetraacetic acid (EDTA), a wetting agent. The constituents are 5% glutaraldehyde and 35% EDTA in the commercial products. Current example products are GLUMA, MicroPrime G, Glu/Sense, and G5 Desensitizer (figure 2).
Two carefully placed one-minute applications suctioned off the tooth after each minute (not washed off) penetrate to the dental pulp, disinfecting and desensitizing the tooth.1 Do not get these materials on the gingiva since they are an irritant.
This glutaraldehyde/HEMA solution is used in the following sequence for a composite restoration:
- Tooth prep
- Desensitizer-disinfectant (used as above)
- Liner, if necessary
- Acid-etch of entire prep
- Bonding agent
- Composite
Select the best category of resin for specific situations
Currently, composite restorative categories are conventional fully filled putty, flowable, bulk-fill, and dual-cure. The type of resin used and the technique of placement are key factors in whether recurrent/continuing caries begins. The following are potential advantages and challenges for each category.
Conventional fully filled putty composite resin
When placed properly, this is one of the best types of resin. The putty consistency makes it relatively easy to manipulate without creating overhangs and overfilling. The high filler content provides optimum strength and wear characteristics.
Challenges present when placing putty composite in increments are:
- Unless allowed to soften with body heat for a few seconds, they can be too thick, which reduces their penetration into relatively inaccessible locations.
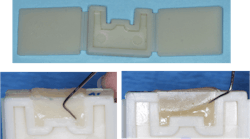
- Their thick viscosity can produce voids between increments called “knit lines” as the increments are placed on top of one another. The clinical significance of this phenomenon is unknown when inside the restorative material, but the voids might possibly be a challenge if on margins. Most experienced dentists and clinically oriented researchers agree that increments larger than 2 mm thick are questionable (figures 3–5).
Flowable composite resin
The popularity of this type of resin for routine use as a total restoration is questionable, but there are some advantages for limited uses.
The flowable viscosity makes it easy to place in tooth preparations. It flows into inaccessible areas on the prep that may be difficult for adequate penetration of putty resin, unless the putty is allowed to warm in the prep to body temperature for a few seconds and pressure is placed on it.
Challenges are the low viscosity and relatively uncontrollable placement of the resin, which often inadvertently creates overfilling. When a prep is overfilled, finishing is more difficult and the well-known “white line” on the prep margins occurs. The white line is an open margin filled with mutilated composite and tooth structure, potentially leading to subsequent caries. Because of the lack of putty characteristic, it can be more difficult to create a tight contact unless an excellent matrix has been applied.
Flowable resins, with only a few exceptions, have higher polymerization shrinkage than putty resins due to having fewer fillers. This leads to even more margin opening than created by the average 2% shrinkage of putty resins (figure 3).
My suggestion is to use flowable resins sparingly: in areas of difficult access for putty, for repair of bis-acryl temporary restorations, and as a replacement for the usually lesser-filled sealants.
Bulk-fill composite resin
As with flowable resins, routine use of bulk-fills for the total restoration is questionable, but there are some good characteristics. Most of these resins have properties that allow deeper penetration of light and potentially more acceptable curing.
Companies promote them for use as larger increments. If lights are used adequately, that suggestion is probably valid, but proper light use by dentists is inconsistent, as we’ll discuss later.
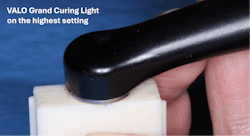
The challenges are like those of flowables. There is a tendency to overfill, requiring longer and more difficult finishing. Unless light curing is done correctly, there is unacceptable resin curing and the potential for caries. My suggestions: Use careful light curing if you are using bulk-fill resins. Aim the light perfectly perpendicular to the resin surface (figure 4). Don’t plan on any time savings if you overfill, and be careful to use a matrix adequately to avoid lack of tight contact areas.
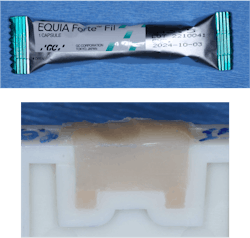
Dual-cure composite resin
Most of the undercuring of composite is in the proximal box forms of class II restorations (figure 5). It makes sense to consider dual-cure resins, which cure chemically and with light. When these are used, the resin is placed in the prep and allowed to chemically cure for a short period followed by conventional light curing. If placed correctly, undercure is eliminated.
Some of the currently available popular brands are:
- Bulk EZ PLUS (Zest Dental Solutions)
- Fill-Up! (Coltene)
- HyperFIL (Parkell)
- Injectafil (Vista Apex Dental)
- LuxaCrown (DMG)
- Stela (SDI)
If lack of adequate curing resin is one of your major challenges, -dual-cure may be your answer.
Summary
It is well proven microscopically that composite margins are open. Composite is not cariostatic. The concepts in this article can reduce or eliminate new caries around and under composite restorations. When you add that information to the use of resin-modified or conventional glass ionomer used as a liner or dentin substitute, you can expect a significant reduction in new caries (figure 6).
Reference
- CR historical perspective on tooth disinfection. Clinicians Report. 2020;13(10).
Editor's note: This article appeared in the April 2024 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, RDH, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.