Solving challenges with zirconia and lithium disilicate crowns
Each month, Dr. Gordon Christensen answers a question from readers about everyday dentistry.
Q: During the last 10 years, I have been using a variety of newer crowns: zirconia, lithium disilicate, and others. I have ceased using porcelain-fused-to-metal (PFM) and cast-gold alloy crowns. Previously, I placed hundreds of crowns using the older materials and techniques. Now, I am seeing some advantages for the newer crowns but also numerous negatives. Have we moved forward or backward with crowns and fixed prostheses, and where are we going?
A: As you know, crowns and fixed prostheses are responsible for a major part of the income for general practices. I am hearing your question often as I speak to large groups of dentists. The common complaints usually include crowns coming off, some of the newer versions of zirconia crowns breaking, occasional breakage of single- and multiple-unit lithium disilicate crowns, fixed prostheses breaking, premature caries on margins, wear of opposing enamel surfaces, as well as other challenges. Research is either completed or underway for each of these issues. To answer your question, I’ll look at some common problems and provide potential solutions for each. For voluminous research information, go to PubMed.
You may also be interested in ... Successful dental restorations: Tips from an industry expert
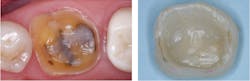
Crowns coming off in service
A frustrating occurrence is crowns coming off in service (figure 1), observed primarily with zirconia crowns. This is a relatively new problem. This phenomenon was almost never observed with conventional glass ionomer or zinc phosphate cements, the most common cements of previous years. The problem appears to relate mostly to the flexibility of resin cements and, to a lesser degree, resin-modified glass ionomer (RMGI) cements.
Zirconia in any of its iterations is a rigid material. The theory being presented is that when a patient bites with an impact on hard zirconia, the flexible resin cement distorts, and the crown comes off. If the tooth preparation is adequate, the problem is usually not present for lithium disilicate restorations because of the hydrofluoric acid etch of the intaglio restoration surfaces.
You may also be interested in ... Successful cementing of zirconia crowns: Still a problem
Potential solution: Consider the tooth preparation and cement used. Comments I hear from practicing dentists indicate zirconia crowns are coming off when crown preparations lack retention. What is a retentive crown preparation? Research shows approximately 4 mm of axial walls from the cervical margin to the occlusal table, with 20 degrees or less deviation from the long axis of the tooth prep (figure 2). Often, this is not possible, especially on mandibular second molars.
When ideal prep characteristics are not possible due to anatomical reasons or previously overprepared teeth, this simple procedure usually solves the problem:
- Make the prep as parallel as possible or build it up to provide more adequate structure.
- On the seating appointment, roughen the tooth preparation’s axial walls and the intaglio surfaces of the restoration with a coarse diamond. This is not a problem with full-strength zirconia (3Y), but it infrequently causes breakage of weaker zirconia restorations (4Y–5Y).
- Seat with either an RMGI (RelyX Luting or FujiCem Evolve, or a conventional glass ionomer cement like Ketac Cem or Fuji One). The rigidity of these cements has been shown to resist crowns coming off better than flexible resin cements.1 When seating with these cements, be sure to use two one-minute applications of glutaraldehyde-containing materials (MicroPrime G, Gluma, or others) to disinfect the tooth preparation and avoid postoperative tooth sensitivity.
Zirconia crowns breaking
The weaker versions of zirconia (esthetic zirconia, 4Y+ zirconia, and other names) have significantly less strength than the original zirconia formulations (full-strength, 3Y, or other names).
Potential solution: When heavy occlusal forces (bruxers, clenchers, or any peculiar situation expected to have heavy occlusal forces on the restoration) are expected, avoid using the weaker versions of zirconia.
Lithium disilicate crowns, anterior fixed prostheses breaking
Lithium disilicate is significantly weaker than any of the current zirconia types. Breakage in service is infrequent, as shown by research.2
Potential solution: For optimum strength, lithium disilicate must be at least 1 mm thick on all restoration surfaces, both axial walls and occlusal surfaces. This is difficult or impossible for small teeth such as maxillary lateral incisors or mandibular incisors.
There is another challenge. Laboratory technicians are currently spacing the digital and analog dies up to 0.5 mm on the external and internal, reducing the overall thickness of both zirconia and lithium disilicate (figure 3).
If you reduce the occlusal surface of the prep 1.5–2.0 mm, the spacing from the lab will cause the ceramic thickness to be reduced 0.5–1.0 mm. Make sure the preps for lithium disilicate and zirconia are made deeply enough to compensate for these laboratory challenges or talk to your lab technician and request less spacing.
More open margins in zirconia, lithium disilicate crowns
The current zirconia and lithium disilicate crowns have margins that are more open than previous generations of crowns made by casting metal. Milling machines cannot make margins fit as accurately as cast-gold or PFM crowns. So what if there are more open margins?
The cements of today vary in their cariostatic properties. Resin cements have no cariostatic properties. Although their composition is the same as composite restorative materials, they have less filler, which causes more shrinkage than restorative resins. The result is the already-open margins are then filled with potentially caries-promoting cement.
Potential solution: Avoid resin cement if possible. Use the well-known cariostatic RMGI or conventional glass ionomer cements described above. Conventional glass ionomer cements have a long history of cariostatic activity, but their use was reduced due to the occurrence of postoperative tooth sensitivity.
This challenge can be overcome by using glutaraldehyde-containing products such as MicroPrime G, Gluma, or others. If these products are used for two one-minute applications before cementing the restorations, postoperative sensitivity will be greatly reduced or even eliminated per TRAC Research.3
An additional advantage: the cement is rigid, which reduces the problem of zirconia crowns coming off.
Matching tooth color is difficult
Current zirconia formulations make matching tooth color difficult (figure 4). Zirconia pucks from which the crowns are milled are not similar in color. For example, an A2 color in one puck can vary significantly from an A2 in another puck. As a result, labs do superficial staining and glazing to make the color adequate. These materials gradually wear off the zirconia base material, as well as wear opposing teeth or restorations while they are on the zirconia.
Potential solution: If this problem occurs with a specific case, ask the lab to avoid staining and glazing on the occlusal surface. Full-strength (3Y) polished zirconia wears opposing teeth like enamel.
Zirconia, ongoing
Although full-zirconia restorations have been used for more than 12 years, they are still an evolving procedure. Changes are constantly being made in zirconia formulations, cements, external staining and glazing, pre-sintering staining, and other factors. Record the zirconia formulations, cements, and other products you are using to validate your own procedures and keep up-to-date with current research.
You may also be interested in ... Occlusion and caries: Ongoing zirconia challenges
Editor's note: This article appeared in the October 2023 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Christensen GJ. How long do dental restorations last? Dental Economics. December 16, 2022. https://www.dentaleconomics.com/science-tech/article/14285541/how-long-do-dental-restorations-last
- TRAC Research. IPS e.max: maximizing its potential and preventing failures. Clinicians Report. July 2019. https://www.cliniciansreport.org/products/dental-reports/clinicians-report-july-2019-volume-12-issue-7
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic.
One-hour videos:
- Strong, Comfortable, Esthetic Rehabilitations with Zirconia (Item #V1942)
- Foolproof, Fast Single Crown Restoration (Item #V1980)
Two-day hands-on courses in Utah:
- Restorative / Esthetic / Preventive Dentistry with Dr. Gordon Christensen
- Fixed Prosthodontics Simplified with Dr. Gordon Christensen
- Simplifying Complex Treatment with Dr .Gordon Christensen
For more information, visit the Practical Clinical Courses website or call (800) 223-6569.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.