Has pulp capping been replaced by endo treatment?
I was out of town recently, and one of my patients had to see another dentist because “a filling had fallen out” of a molar tooth. When I returned, I was shocked to see that the dentist had performed a root canal, a post and core, and a crown for nearly $3,000. The patient was quite frustrated with the complexity of the treatment.
I looked at the previous radiographs of the molar site. The tooth had a minimal-sized old amalgam in it with slightly questionable potential caries on the box form that had been present radiographically for several recare appointments. It appeared that the dentist completed more treatment than was necessary. Even if the caries was close to the pulp, a pulp cap would have been indicated. What has happened to conservative dentistry?
More from the author ...
Critique of dental procedures and potential solutions
How long do dental restorations last?
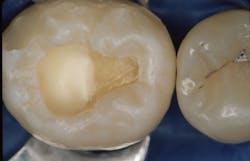
I often see similar situations, and I am equally concerned that overtreatment has been or is being done. Currently, there appears to be more endodontic treatment on teeth that could have been treated much more conservatively (figure 1). There is also some uncertainty among dentists about whether to place posts in teeth when endodontic treatment has been accomplished, which is an entirely different question. I will limit my answer to some suggestions about preserving the dental pulp with indirect or direct pulp caps based on both international research and my own experience over many years.
Indirect pulp capping
This procedure should be a near-daily treatment in most general practices. What is an indirect pulp cap? There is some confusion among dentists. An indirect pulp cap is identified when caries has progressed to the point that it is very close to the pulp; there may even be pink color in the dentin testifying to this situation. How should this be treated (figure 2)?
- Inform the patient about what you are going to do. Provide information that the pulp capping procedure usually works well, but there is a minimal chance root canal treatment may be needed.
- Provide a dry field with a rubber dam (Isolite 3, Mr. Thirsty, or others).
- Remove the external portion of the caries until all the peripheral walls of the cavity prep are clearly free of caries.
- Continue to remove caries on the internal dentin surfaces until the dentin is hard and any further removal would be difficult. Don’t remove discolored dentin unless it’s soft. It will be disinfected in the next step.
- Disinfect the tooth. According to research at Clinicians Report Foundation TRAC department1 accomplished over many years, glutaraldehyde-containing products such as Zest Dental Solutions’ MicroPrime or Kulzer Gluma (5% glutaraldehyde and 35% HEMA) both disinfect and desensitize dentin. Clinical research and patient comments validate the desensitization, and empirically observed reduction in subsequent caries indicates disinfection of the tooth. Some companies don’t prefer glutaraldehyde-containing solutions to be used for this procedure, stating that these solutions can cause damage to the gingiva. That is correct. Many chemicals used in dentistry and other medical specialties irritate or damage soft tissues. Just don’t let the solution get on the soft tissue. Use a small microbrush, like those usually used to place bonding agents or medications on teeth, with a minimal amount of solution. Place the glutaraldehyde solution on the tooth preparation and allow it to remain for one full minute. Refresh the solution for one more minute (a total of two minutes). This procedure allows the glutaraldehyde solution to penetrate completely to the pulp, coagulating the dentin, closing the dentinal tubules, and disinfecting the tooth preparation. Do not wash the solution from the tooth surface; just suction the excess off with high-velocity suction.
- Place your choice of pulp capping material for the indirect pulp cap. See the direct pulp capping section below for some differences when blood is present. Currently, either resin-modified glass ionomer (RMGI; 3M Vitrebond Plus, GC Fuji Lining, or others) or mineral trioxide aggregate (MTA; Ultradent Products Endo-Eze MTAFlow or others) are two very popular materials for pulp capping. There are many others, and most seem to work well.
- If MTA is used in step 6, some dentists prefer to place a layer of light-cured RMGI over the MTA, which provides some rigidity and can make placement of the restorative material easier.
- Acid-etch the tooth preparation with your preferred procedure (total etch, selective enamel etch only, or self-etch).
- Place and cure the bonding agent of your choice.
- Place and finish the restorative material of your choice.
- Inform the patient about what you expect postoperatively, which is usually nothing.
This indirect pulp capping procedure has been researched for many years and has had the empirical acceptance of thousands of dentists relative to its effectiveness.
Direct pulp capping
Deeper caries requiring direct pulp capping don’t require a procedure significantly different from the one described for indirect pulp capping. What is a direct pulp cap? Steps 1–6 of the indirect pulp capping technique are nearly identical to those of the direct pulp capping technique, with the differences listed below. These suggestions are empirical. There is not much evidence-based research on when a direct pulp cap should be done. More information can be gleaned from the many articles on this subject.
- The younger the patient, the greater the success (which would be expected).
- The pulp penetration should be small—i.e., not more than 1 mm in diameter.
- The dentin around the penetration should be hard.
- Blood coming from the penetration should be normal-looking red blood, slowly flowing, and not rushing out (which would suggest a hyperemic pulp).
- The blood flow can be controlled by using typically suggested materials placed on a cotton pellet: ferric sulfate, saline, sodium hypochlorite, hydrogen peroxide, and chlorhexidine. If the blood flow cannot be controlled within three seconds with ferric sulfate (Ultradent Products Astringedent), try one more time. If the blood flow still cannot be controlled, the tooth may be hyperemic, which would reduce predictions of clinical success.
- Place the glutaraldehyde solution as in step 4 above, directly on the pulp penetration.
- The remaining steps 6–11 are the same for a direct pulp cap, with the exception that the prediction for success should be reduced.
- From evidence-based studies, the success of direct pulp capping is estimated to be around 60%. But the studies are not equal in design, nor do they have the same techniques or the same follow-up time. It is my personal experience after doing hundreds of direct pulp caps that the success is higher than 60%.
- Studies on indirect pulp caps are similarly confounded. From my years of experience, I estimate the success of indirect pulp caps to be significantly higher than that of direct pulp caps.
Summary
Indirect and direct pulp capping are well-proven ways to avoid doing endodontics on teeth with deep caries. Clinicians should consider conservative restorative dentistry for suspect teeth, rather than endodontics.
Reference
1. Commonly asked questions about use of glutaraldehyde/HEMA. How to predictably reduce post-op tooth sensitivity and caries. Clinicians Report. 2020;13(10).
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic.
One-hour videos:
- Making Foolproof Class II Composites (Item #V3501)
- Mastering Frequent Esthetic Challenges with Resin (Item #V3582)
Two-day hands-on courses in Utah:
- Restorative / Esthetic / Preventive Dentistry with Dr. Gordon Christensen
- Simplifying Complex Treatment with Dr. Gordon Christensen
For more information, visit Practical Clinical Courses or call (800) 223-6569.
Editor's note: This article appeared in the May 2023 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.