Comparing new vs. older dental concepts
Q: It seems as if new concepts, techniques, materials, and technologies are coming so fast in dentistry that it’s difficult to determine when to change to a new one or stay with what I have always used. Some of the new procedures seem to be more difficult and expensive. Do you have some suggestions for me?
A: I have been out of school for many years. There is not a significant amount of information from dental school that I still use today. Change is constant. I’ve selected a few of the most important recent changes and will delve into the techniques that are clearly more adequate than older concepts and those that are not. Included are the advantages and disadvantages of each as well as my suggestions concerning which concepts are best, based on both research and clinical observation.
More from the author ...
Occlusion and caries: Ongoing zirconia challenges
Increase your service and revenue with elective dental procedures
Restoring a tooth versus removing the tooth and placing an implant
When root-form implants were first introduced to the profession more than 30 years ago, it was thought that they would eventually be proven to be better than natural teeth. Has that happened? In the first few years, they looked excellent with very few failures. Now, 30-plus years later, the incidence of peri-mucositis and peri-implantitis are showing estimates that nearly one-half of implants have peri-implantitis, and some must be removed.1,2
Comparison: Natural teeth move in bone in direct relation to masticatory muscle forces and occlusion. Implants do not move. When implants are placed in situations where natural teeth are surrounding them, the occlusion changes significantly. Often, contact areas open as the natural teeth move and the implant does not. Food impactions and subsequent periodontal problems occur. The now known periodontal breakdown—peri-implantitis—is a growing threat.
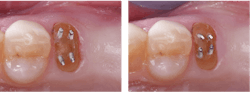
Conclusion: Retention of a restorable broken-down tooth is the best solution, when possible (figure 1).
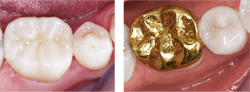
Cast-gold alloy crowns versus zirconia crowns
Cast-gold alloy restorations have been used since the early 1900s. Their service potential is well known and respected by dentists and patients. Statements and studies about gold crowns serving more than 40 years are commonly reported by dentists. However, the current desire for white teeth has reduced patient acceptance of gold as a restorative material. The cost of gold alloy and the significantly longer laboratory time to make gold alloy restorations have reduced their use to only about 2% of crowns in the US (personal communication, Darryl Withrow, Glidewell Laboratories).
Comparison: The following statements are from various in vivo research projects by TRAC Research (Technologies in Restoratives and Caries Research) of Clinicians Report Foundation and can be found online at cliniciansreport.org. Cast gold alloys vary in hardness and wear resistance. If the proper alloy formulation is used and the clinical technique is correct, cast gold wears nearly like tooth enamel and is not abusive to opposing teeth. Zirconia (3Y, class 5, tetragonal zirconia) polished, without glaze, also wears very similarly to tooth enamel. 4Y, class 4 and higher, cubic zirconia has been shown to wear opposing teeth and has lower strength than tetragonal zirconia. The cost and time involved in making zirconia crowns is far less than the cost of making gold alloy crowns, and some types of internally stained zirconia crowns can simulate optimum tooth color. The margins of milled zirconia crowns are at least twice more open than gold alloy crowns. Many zirconia crowns have been reported to come off in service. Zirconia crowns are best cemented with resin-modified glass ionomer (RMGI) cement for its cariostatic properties and proven better retention. Resin cement has no cariostatic properties and is flexible, causing release of zirconia crowns more often than RMGI cement.
Conclusion: Currently, over 90% of crowns made in the USA are zirconia or lithium disilicate, and about 80% of the 90% total are zirconia. Zirconia is growing faster than lithium disilicate, probably because it is easier to make in the laboratory and less expensive (personal communication, Darryl Withrow, Glidewell Laboratories). Although cast gold is great, its use is currently minimal. Refinements in zirconia formulation and color predictability are still needed. Zirconia of the right formulation, cemented correctly, is the closest restoration to cast gold in its properties of any previous restorative material. Zirconia of various formulations continues to dominate the market, and its use will only increase (figure 2).
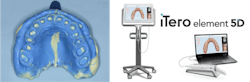
Vinyl polysiloxane or polyether versus scanning
Scanning is one of the fastest-growing dental technologies today. Scanners have been used for more than 30 years and have finally caught on with dental practitioners. Large laboratories estimate that scanned impressions comprise about 30%–40% of all impressions for crowns, with vinyl polysiloxane or polyether comprising the remainder.
Comparison: Current scanners are expensive, large, inaccurate for long spans, require a learning period, and overall are less accurate than vinyl polysiloxane or polyether. But their relative ease of use and patient preference continues to stimulate their growth in the market (figure 3). Scanning technology is in an evolutionary period. It is still an elective technology, since conventional impressions are less expensive, well-known, and more accurate.
Conclusion: Despite their evident disadvantages, scanners have many advantages. Some of them are easy delegation to staff, large monitor and image known to increase quality of preps, lack of debris on the patient, good patient acceptance, few infection control challenges, and ability to store data for future use. Scanners are the future, but the disadvantages are evident; manufacturers need to modify scanners to reduce or eliminate those. Don’t throw away elastomer impressions just yet.
Aligners versus conventional orthodontics
Clinicians Report was one of the first research groups to evaluate aligners many years ago.3 The original research and development of aligners was done by computer experts evaluating basic science information on the best methods to move teeth in bone. Later, many dental laboratories started making aligners. Some labs provided education for dentists, while others did not follow up on how the aligners were used, causing some clinical challenges.
Comparison: Dentists who have been adequately educated in aligner treatment and who educate patients and follow up carefully can treat many simple-to-moderate malocclusions. However, inadequate education of dentists and patients on how to use aligners has resulted in unfortunate clinical problems when teeth are moved too rapidly (figure 4).
Conclusion: General practitioners wanting to provide aligner treatment for their patients should seek comprehensive continuing education first, educate their staff about the treatment, and follow up thoroughly with patients as the treatment progresses. Go to pccdental.com for information on a two-day course on orthodontics for GPs.
Final conclusions
This comparison of four example areas in dentistry where historic techniques are being challenged by new techniques demonstrates that just because something is new doesn’t always mean it’s better. In some situations, new procedures may be worse and more expensive to accomplish than the historic ones. There are many exciting and successful techniques and materials, and only you can decide if they will be desirable for your patients.
Editor's note: This article appeared in the March 2023 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Why are implants failing? Clinicians Report. 2021;14(9).
- Clinicians Report. 2023;16(2).
- Clear orthodontic aligners: the right option for your patients? Clinicians Report. 2021;14(6).
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic.
One-hour videos:
- Strong, Comfortable, Esthetic Rehabilitations with Zirconia (Item #V1942)
- Cementing Restorations—Proven and Successful (Item #V1921)
Two-day hands-on courses
in Utah:
- Faster, Easier, Higher Quality Dentistry with Dr. Gordon Christensen
- Simplifying Complex Treatment with Dr. Gordon Christensen
For more information, visit pccdental.com or contact Practical Clinical Courses at (800) 223-6569.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.