Successful cementing of zirconia crowns: Still a problem
Q: I have cemented many zirconia crowns, but some are still coming off during service. I have done what some of the companies have recommended for this problem, and the crowns are still coming off. This challenge almost never happened with some of the older generations of cement. What can be done about this significant problem?
A: You and tens of thousands of other dentists are having the same problem. Your statement is not new information. This problem has been observed for about 11 years, since zirconia crowns were first introduced to the profession, and it continues to be reported routinely by dental practitioners.
Zirconia crowns are the most popular crown type in the US (figure 1). What can cause the disagreeable situation of crowns coming off? Here are the most important reasons:
Tooth preparation. Many studies have been conducted to determine tooth preparation characteristics that produce optimum retention. If the preparation is for a tooth that was not previously prepared for a crown, the ideal characteristics are easily defined (figure 2). The axial walls of the prep should have 4 mm or more of sound tooth structure or secured buildup material from the cervical margin to the occlusal table on all four axial walls. The prep should have no more than 20 degrees of taper from the tooth’s long axis. These characteristics are often not possible if the tooth has not fully erupted or is in a location (such as mandibular second molars) with only short clinical crowns present. The solution to this condition will be discussed later.
Teeth having been previously prepared for a crown with more than 20 degrees of taper are observed often when redoing tooth preparations for new crowns.
Teeth requiring significant buildup of the coronal portions can be rebuilt to near-optimum characteristics, but as is observed in dental laboratories, often dentists do not build them back to normal tooth anatomy, increasing the possibility that crowns will come off due to lack of retention.
Other problems somewhat unrelated to crown retention but still highly important are inadequate occlusal reduction and lack of anatomical characteristics prepared into the occlusal surfaces.
Many labs are making excessive spacing on both the internal of crowns and the external of the occlusal surface, significantly reducing the amount of zirconia on the occlusal surface of the crown. Why do they do this? The crown seats easily and the occlusal surface does not require zirconia removal. But excessive spacing weakens the crown!
Most dental laboratories report routine observation of inadequate tooth preparations.
Physical properties of cements. The material holding the crown in place should be rigid. Some resilient dental materials, such as resin cements, are being promoted by manufacturers for zirconia crown cementation using the reasoning that resin cements are stronger than resin-modified glass ionomer (RMGI). They are correct; resin is the strongest. However, resin is flexible. With this flexibility, inadvertent biting on a hard object can potentially flex the cement and dislodge the crown.
You were correct in stating that older cements did not allow crowns to come off in service. Consider zinc phosphate or conventional glass ionomer. Neither cement had significant flexibility, and the crowns almost never came off.
The TRAC (Technologies in Restoratives and Caries Research) component of Clinicians Report Foundation has studied this problem in depth. Over various periods of clinical service, TRAC evaluated three categories of cement in vivo for zirconia crowns: adhesive resin, self-adhesive resin, and RMGI. Seven brands of cement and 14 brands of zirconia were included in the study.
- One percent of RMGI cemented crowns have debonded over the length of the study to date.
- Four percent of resin adhesive cemented zirconia crowns debonded.
- Five percent of resin self-adhesive cemented crowns debonded.
This study is still underway, but clearly, the zirconia crowns cemented with resin cements have debonded more than crowns cemented with RMGI. Although there could be other reasons for the differences among the three types of cements, a logical tentative conclusion is that the resiliency of the resin cement caused the debonding more than the rigid RMGI. This tentative conclusion refutes the suggestion of some manufacturers that the stronger resin would produce greater retention.
Improving retention of zirconia crowns
Consider these clinical suggestions to address retention:
- When possible, make the tooth preparation according to previous suggestions.
- When one-half or more of the coronal tooth structure is gone, increase the remaining tooth strength by building it up with strongly secured composite resin to allow for the prep anatomy described above.
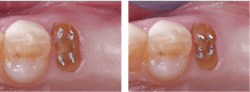
- Use retentive pins when necessary for retention of the buildup material. Place each pin at least 15 degrees from the long axis of the tooth (examples of titanium pins: Stabilok Dentin Pins or Filpin Pins (figure 3).
- Use a good bonding agent such as 3M Scotchbond Universal Plus or Kuraray Clearfil Universal Bond Quick.
- For short preps or those with too much taper (or both), increase the mechanical crown retention by having your technician place horizontal grooves in the intaglio surfaces of the crown in the presintered zirconia.
- For short preps or those with too much taper (or both), increase the mechanical retention on the prep by placing horizontal grooves on all four axial walls with a coarse diamond.
- The combination of numbers four and five on this list strongly reduce or eliminate the crown coming off in service.
- Avoid using resin cement for zirconia crowns.
- Use RMGI cement (3M RelyX Luting Plus, GC FugiCEM Evolve, or other RMGIs).
- Make sure occlusion is not too high and that excursive movements are not providing occlusal interferences.
- Regardless of the crown type, tell patients to avoid eating sticky or hard foods. When necessary, they can allow the sticky or hard food to dissolve or soften in their mouth rather than biting down hard on it.
Additional tips for increasing clinical longevity of zirconia crowns
Zirconia crown margins are open far more than cast gold alloy margins, which necessitates extra preventive care.
Ensure that the patient is using at least standard fluoride toothpaste. Most OTC toothpastes contain 1,000 ppm fluoride.
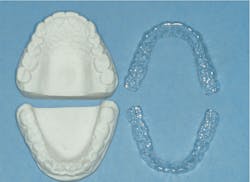
If the patient is considered to have high-caries activity, place them on Colgate PreviDent 5000 Booster Plus used as a thin strip of material on a toothbrush, or PreviDent 5000 Gel in trays for two five-minute periods each day after breakfast and just before bed (figure 4).
Summary
The frustrating challenge of zirconia crowns coming off continues to be a significant problem in dentistry. Follow the methods discussed in this article to reduce or eliminate the problem.
Editor's note: This article appeared in the January 2023 print edition of Dental Economics magazine and was updated as of November 2024. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic:
One-hour videos:
- Strong, Comfortable, Esthetic Rehabilitations with Zirconia (Item #V1942)
- Cementing Restorations—Proven and Successful (Item #V1921)
Three-hour virtual courses:
- Christensen’s Most Frequent Failures and How to Avoid Them (Item #X4740)
- Making Occlusion Work for Your Practice (Item #X3145)
For more information, visit pccdental.com or contact Practical Clinical Courses at (800) 223-6569.Courses at (800) 223-6569.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.