Mitigating composite shrinkage in restorative dentistry
A rarely discussed contradiction in restorative dentistry is the immense popularity of resin composite restorations, despite current evidence suggesting amalgam has a better longevity than resin composites for posterior restorations.1 While clinical longevity is important, these studies don’t account for the fact that perhaps the greatest advantage of resin composite restorations is that they allow practitioners to design their tooth preparations more conservatively, as the restorations may be retained with adhesive bonding rather than mechanical retention. Conservative tooth preparations may allow preservation of tooth structure for both placement of new margins during repair or replacement and conservation of the structural integrity of the tooth. Additionally, a more conservative tooth preparation may avoid the dental pulp.
The success of resin composite restorations is dependent on overcoming two critical challenges: (1) achieving an adhesive bond to tooth structure, and (2) managing the inherent polymerization shrinkage of resin composites. In this article, we will address the shrinkage of dental composites and suggest techniques to minimize its negative clinical outcomes.
Why does resin composite shrink?
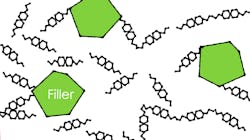
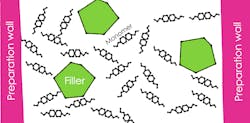
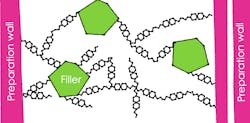
The “resins” in dental composites, adhesives, and cements are typically various
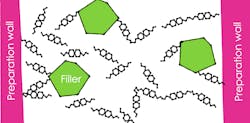
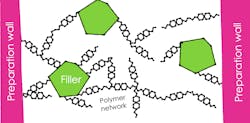
and cross-linked networks that the resin composite transforms from a viscous substance to a solid, the material is said to have reached its gel point (figure 3). Elimination of intermolecular spacing in post-gel point polymerization leads to the development of shrinkage stress (figure 4).
Additional reading: Combining glass ionomer, IDS, and CEREC for intelligent hybrid restorations
In which direction does composite shrink?
Does composite shrink toward the light or toward the bonded walls of the tooth? Although an often-taught concept is that resin composites shrink toward the curing light, a better explanation is that resin composites flow toward the direction in which they are being pulled. For nonbonded composites, the
Imagine a large piece of fabric lying on the floor of which you bunch together a small section with your fist. The fabric will move toward the direction in which the bunching is occurring. Similarly, the composite should shrink toward the light as there is a higher light intensity and increased rate of conversion of the resin near the surface of a curing light.
An alternative theory is that resin composite will be pulled toward bonded surfaces. Finite element modeling of bonded, light-cured resin composite restorations showed that shrinkage vectors were directed toward the bonded boundaries of the tooth preparation.2
A contemporary study presented an elegant model for measuring the actual directions of the shrinkage of bonded resin composites.3 In this model, bonded resin composite restorations were examined with microCT (like 3D radiographs) before and after light polymerization. The filler particles were traced radiographically to determine the direction the material moves during polymerization.
The study reported that material at the unbonded occlusal surface moved toward the center of the restoration due to formation of a meniscus on the occlusal surface. The material in the base of the preparation, however, moved occlusally toward the direction of the curing light. It is unclear if the movement of the composite in the base of the preparation is due to shrinkage toward the light (slower reaction in the base of the preparation) or due to a weaker bond at the base of the preparation (insufficient light for adequate bond). Therefore, shrinkage direction may not be completely elucidated.
If composite in fact shrinks toward the curing light, the directed-flow curing technique is one in which resin composite is cured through the walls of the tooth preparation to direct flow of the polymerizing composite toward the preparation walls.
If composite shrinks toward the walls of the preparation, there is a theory that resin monomers will flow toward the surfaces that can achieve the fastest bond. This hierarchy of bondability theory deduces that bonds develop fastest in enamel, followed by superficial dentin, then deep dentin, and finally affected and infected dentin.4
For example, a layer of composite bonded in a preparation with walls in enamel and dentin would pull material from the dentin to the enamel due to the faster development of the enamel bond. A clinical solution to this problem would be to place composite layers to avoid connection of surfaces with different bondability and allow time for the bond to occur with the slower-bonding surfaces prior to connecting them with faster-bonding surfaces. One clinical practice is to wait five minutes prior to connecting an initial layer of flowable composite on deep dentin with the second layer on more superficial dentin.
Should composites be placed in bulk or increments?
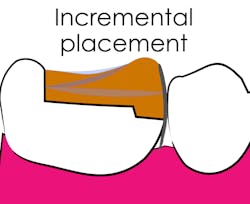
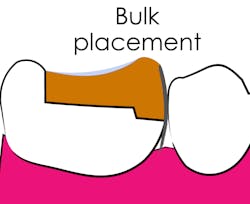
One justification for the bulk placement of composite resin is that 1% shrinkage of a 4 mm increment of composite is the same as 1% shrinkage of four 1 mm increments. This justification neglects the opportunity to form a meniscus on the unbonded surface of each layer of composite. The formation of the meniscus on the unbonded surface allows movement of material in post-gel point polymerization without stress development. Therefore, placement of composite in increments to maximize the amount of unbonded surface area should allow stress relief (figures 5 and 6).
Incremental placement of composite has been criticized due to the ability of shrinking bonded composite to pull together the walls of a tooth preparation. Each increment of cured composite would have the opportunity to pull the walls of the tooth preparation closer together.6
A recent review of both clinical and laboratory studies concluded that no differences could be determined in the marginal adaptation and clinical performance of resin composites placed in layers or in bulk.7
What is a low-shrinkage-stress composite?
One strategy to overcome shrinkage is to use low-shrinkage-stress composite. An important differentiation should be made between volumetric shrinkage of composite (reported as a %) and shrinkage stress (reported in MPa). A composite may undergo a large amount of volumetric shrinkage when placed in an unbonded preparation yet apply a relatively low amount of shrinkage stress to the walls of a bonded preparation. For example, think of the difference in stress that would be applied on two hooks if a rubber band was stretched one inch between them or a similar-sized automotive spring was stretched the same one inch.
Several approaches have been used to reduce shrinkage stress of resin composites. One approach was to slow the polymerization reaction of the material to allow more time for the composite to flow toward the bonded walls of the preparation prior to reaching its gel point. This concept is a rationale for using chemically cured resin composites that polymerize slower than light-cured resin composites. Additionally, this period of flow can be used to justify delayed light curing of dual-cured restorative materials. Slowing polymerization is also the theory behind ramp or pulse light curing.
Another method to reduce polymerization shrinkage stress is to use low-modulus composites. Low modulus can be thought of as high flexibility. If a resin composite is more flexible, it will apply less stress when stretched during post-gel point polymerization. The disadvantage of using a composite with a modulus lower than the surrounding tooth is that the composite may deform more than the tooth in occlusal function. The differential deformation could lead to stress at the bond interface.
Resins have been developed that can undergo addition fragmentation, a process by which resin polymers experiencing stress at their bonds can break and reform new bonds in a more relaxed arrangement.8
Summary
Several strategies exist for mitigating polymerization stress, including directing the flow of composite with the curing light, disconnecting layers of composite bonded to different substrates, maximizing free surface area in increments of composite, and using composites with prolonged polymerization rates, low modulus, or additional-fragmentation capability.
References
- Moraschini V, Fai CK, Alto RM, Dos Santos GO. Amalgam and resin composite longevity of posterior restorations: a systematic review and meta-analysis. J Dent. 2015;43(9):1043-1050. doi:10.1016/j.jdent.2015.06.005
- Versluis A, Tantbirojn D, Douglas WH. Do dental composites always shrink toward the light? J Dent Res. 1998;77(6):1435-1445. doi:10.1177/00220345980770060801
- Cho E, Sadr A, Inai N, Tagami J. Evaluation of resin composite polymerization by three dimensional micro-CT imaging and nanoindentation. Dent Mater. 2011;27(11):1070-1078. doi:10.1016/j.dental.2011.07.008
- Alleman DS, Alleman DS, Deliperi S, Aravena Diaz J, Martins L, Keulemans F. Decoupling with time. Inside Dent. 2021;17(8):35-40.
- ADA Clinical Evaluator Panel Report. Posterior Composite Restorations. American Dental Association. 2018. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/ace/ace_panel_posterior_composite_restoration_study_-march_2018_2nd_report.pdf
- Bicalho AA, Valdívia AD, Barreto BC, Tantbirojn D, Versluis A, Soares CJ. Incremental filling technique and composite material—part II: shrinkage and shrinkage stresses. Oper Dent. 2014;39(2):E83-E92. doi:10.2341/12-442-L
- Ferracane JL, Lawson NC. Probing the hierarchy of evidence to identify the best strategy for placing class II dental composite restorations using current materials. J Esthet Restor Dent. 2021;33(1):39-50. doi:10.1111/jerd.12686
- Shah PK, Stansbury JW, Bowman CN. Application of an addition-fragmentation-chain transfer monomer in di(meth)acrylate network formation to reduce polymerization shrinkage stress. Polym Chem. 2017;8(30):4339-4351. doi:10.1039/C7PY00702G
Editor's note: This article originally appeared in the February 2022 print edition of Dental Economics.
About the Author
Nathaniel Lawson, DMD, PhD
Nathaniel Lawson, DMD, PhD, is an associate professor and the director of the division of biomaterials at the University of Alabama at Birmingham School of Dentistry. He graduated from UAB School of Dentistry in 2011 and obtained his PhD in biomedical engineering in 2012. He has lectured internationally, served as an investigator on numerous research grants, and published extensively on dental materials. He also works as a general dentist in the UAB Faculty Practice.
Updated September 25, 2023
Augusto Robles, DMD, MS
Augusto Robles, DMD, MS, is the director of the Operative Dentistry Curriculum at the University of Alabama at Birmingham School of Dentistry and a visiting instructor at the Dawson Academy.
Updated December 28, 2021