Q: I have been placing dental implants for more than 10 years and carefully observing the crowns and fixed prostheses I have placed on them. Most of the restorations look nearly like they did when placed on the implants, but some of the implants have obvious radiographic signs of advancing peri-implant mucositis and peri-implantitis. I am quite concerned about what I am seeing. I have a candid question for you: If you had a missing tooth yourself, would you prefer an implant and a crown or a three-unit fixed prosthesis?
A: Thanks for your highly important and timely question. I have been placing implants for about 30 years. When they were first available, most of us thought we had a replacement for teeth that might be better than the actual teeth. After about 10 years, we started to doubt that statement in some cases, as the bone started to degenerate and expose the implant surface, caused by what we now call peri-implantitis. Several years later, we saw some implants fail to the degree they had to be removed. These failures refuted the approximate 95% success rate reported in many studies shortly after the implants were placed. Apparently, you have also observed these maladies. Do we know why implants fail? Yes, in a few situations, and no in most others.
Am I negative about implants and their success? Absolutely not! The profession now has many studies reporting the alleged reasons for the challenges we have observed. Except for some obvious situations, nobody really knows the exact reason for implant failure, but we certainly have numerous speculative and apparent reasons.
SOME POSSIBLE reasons for implant failure
The following topics have reported research projects relating them to implant failure. You may go to PubMed, Google Scholar, Cochrane Collaboration, or other sites to see for yourself. I will list each item along with a very brief statement. They are not in any prioritized order.
Metal allergies. You may think nobody has any physical challenges with the elements in most implants: titanium, vanadium, or aluminum. You are wrong. A small percentage of the population have allergic reactions to the metal implants themselves.
Previous periodontal disease. Early in the profession’s experience with implants, many thought that periodontal disease disappeared when the teeth were removed. That has since been disproved. Make sure you find out about previous periodontal disease in your patients before placing implants and proceed cautiously.
Radiation. Head or neck radiation has an alleged negative influence on implants. Significant radiation is now considered to be a risk for implant failure.
Oral hygiene. Most potential implant patients have lost their teeth due to many factors, but inadequate oral hygiene is one of the most common reasons. Their oral hygiene behavior is not likely to change, since they may believe their dental problems are over when implants are placed. Microbes present in periodontal disease are on the list as a potential reason for peri-implantitis and implant failure.
Diet. Does chewing hard foods on a newly placed implant influence osseointegration? Although significant differences regarding food choices or nutrients and implant success are not reported, early loading of the implants and chewing hard foods too aggressively may have a negative influence on osseointegration. The literature suggests that there is a critical threshold of micromotion above which osseointegration may be overcome by encapsulation of the implant.
Systemic disease. There are numerous systemic disease conditions that have been studied relative to implant failure, and there is controversy in the literature. Other conditions and situations have had some negative reports including:
- Recent myocardial infarction
- Recent cerebrovascular accident
- Valvular prosthesis surgery
- Active treatment of a malignancy
- Intravenous bisphosphonate use
- Psychiatric illness
- Drug abuse
- Bleeding issues
- Immunosuppression
- Uncontrolled diabetes
- Smoking
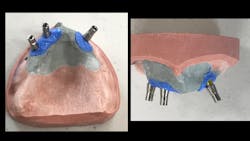
Improper implant placement. This is an extremely important factor. Placement of implants in locations where they receive abusive occlusion or excessive loading is inviting failure (figures 2–4).
Inadequate bone quantity or quality. Inadequate bone quantity is readily observable on radiographs, but inadequate bone quality may not be so apparent. When inadequate bone quality is suspected, the patient should be questioned about the presence of osteopenia or osteoporosis. Most cone beam devices have ability to provide some evidence of lack of bone density, but the numerical observation of bone density scores on cone beam devices should be used with caution. If bone density is questionable and unknown, a T-score bone density test should be scheduled and evaluated before deciding to place implants.
Poorly designed prosthesis. Practitioners placing implants should have significant knowledge of prosthodontics. When implants are placed in incorrect locations, both proper loading of the implants and development of an optimal esthetic result are compromised.
Loading too early. This is a controversial factor. Significant research supports this concept, but there are also reports showing preference for implant placement in mature bone. There are some significant, positive, esthetic advantages for immediate loading, but other factors should be considered before deciding upon this approach.
Microbes. The mouth is a virtual reservoir of microbes. Although some researchers have attempted to locate and identify potential microbes responsible for peri-implantitis and peri-implant mucositis, conclusions are yet to come forth on this subject.
These are only a few factors that need to be considered when deciding whether to place implants or use conventional dental procedures such as fixed or removable appliances.
Summary
Dental implants are among the most important and useful innovations ever introduced into dentistry. However, the advent of peri-implant mucositis and peri-implantitis has been a significant occurrence and impediment in recent years. These disease conditions have multifactorial causes, several of which are identified in this article. Diagnosis and treatment planning for implant placement should include a careful consideration of these factors and thorough explanation of each to patients before deciding to place implants. In many cases, conventional restorative procedures may be better than placing implants.
Author’s note: These educational materials from Practical Clinical Courses offer further resources for you and your staff.
One-hour videos:
- Diagnosis and Treatment of Failing Implants (Item no. V2391)
- Simple, Inexpensive Implant Placement—Guide or No Guide? (Item no. V2373)
Two-day hands-on course in Utah:
- Avoiding Implant Failures and How to Treat Them with Drs. Jon Suzuki, Kevin Suzuki, and Gordon Christensen
One-day course in Las Vegas:
- Paradigm Changes in the Profession—2021 with Drs. Gordon and Rella Christensen, Gerry Niznick, Harald Heymann, and Michael LeBlanc on September 18, 2021, at the Mirage Las Vegas.
For more information, visit pccdental.com or contact Practical Clinical Courses at (800) 223-6569.
Editor's note: This article appeared in the August 2021 print edition of Dental Economics.
Gordon J. Christensen, DDS, PhD, MSD, is a practicing prosthodontist in Provo, Utah. He is the founder and CEO of Practical Clinical Courses, an international continuing education organization founded in 1981 for dental professionals. Dr. Christensen is cofounder (with his wife, Rella Christensen, PhD, RDH) and CEO of Clinicians Report.