Q: In spite of how well I may accomplish a typical composite restoration, recurrent caries is commonly present on many of them after a few years. Why don’t manufacturers develop preventive restorative materials? I have tried various glass ionomers (GIs) over the years, but they are difficult to place, and some have failed soon after placement. What can I do to help my restorations last longer?
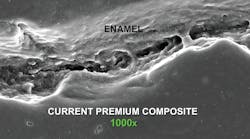
A: I have been practicing for many years and have seen exactly what you describe. Clinically, resin-based composite looks very good for a while, but it soon begins to degenerate and often has caries. As you know, composite has significant shrinkage on polymerization (an average of 2% for most brands), and the margins are wide open to an electron microscope. There is nothing you can do to eliminate the open margins (figure 1). The restorations may look closed to the naked eye, but that is an incorrect assumption.
Until recently, there was not much you could do to improve the caries challenge with resin without changing to older GI materials that have difficult placement characteristics. But that is changing! Dental manufacturers have heard our frustrations, and numerous companies are working on new cariostatic materials yet to be marketed.
In the meantime, there are several significantly changed and improved cariostatic conventional GIs and resin-modified glass ionomers (RMGIs) that need your attention.
What has changed with conventional GIs?
The negative characteristics of older GIs have limited their use:
They were sticky, which made them extremely difficult to place without the placement instrument pulling the restorative material out of the prep. This problem has been reduced markedly for conventional GIs, allowing clinicians to place the material, wait a few seconds, and then pack it into the prep as a putty, similar to a composite. Example brands with this improvement are 3M’s Ketac Universal, GC’s Equia Forte or Equia Forte HT, and Voco’s IonoStar Plus. This is one of the most important characteristic changes in the newer forms of conventional GIs.
Previous conventional GIs set too slowly for most practitioners working in busy practices. This characteristic has also been improved. Although these autoset, chemical-cure materials are not as fast-setting as light-cured resin-based composites, they set much faster than previous versions. This characteristic, along with their higher strength, allows them to be placed in small tooth preparations for children and adults, with the assurance that they will not only be cariostatic, but will also serve for a moderate period of time. The clinical longevity of any GI is not as long as some other materials. This is both good and bad. It’s good because the GI dissolves and releases fluoride into the tooth structure. It’s bad because it loses its original morphology. Later in this article, I will demonstrate how to overcome this problem while still retaining the cariostatic property.
The strength and surface hardness of older GIs were lower than desirable, allowing chipping and clinical degeneration to occur over a relatively short period of time. Again, this characteristic has been improved but not yet eliminated.
The esthetic qualities of older GIs were not high enough for optimum patient acceptance. Although companies have improved this characteristic somewhat (for example, with GC’s Equia Forte HT), GIs are still not equal to the esthetic level of composite resin. This negative characteristic can be overcome completely by using the well-known sandwich technique, which I will discuss later.
What has changed with RMGIs?
Because of their easier handling and partial light-curing characteristics, RMGIs are accepted by more dentists than the older conventional GIs. Twenty percent of RMGI material is resin, which allows this part of the material to be light cured. Because of this, the materials can be placed and finished faster. However, thischaracteristic has not been changed in the newer products. Some of them have quite a high fluoride release, as shown by the TRAC Research department of Clinicians Report Foundation (CR). The most significant improvement in this category of restorative materials is the automixing characteristic introduced by GC in its Fuji Automix LC product (figure 4).
What are the suggested uses of GIs and RMGIs?
Complete filling of small class I, II, III, and IV tooth preparations—Small tooth preparations can be restored completely with GIs. Although this has been done previously by many dentists, especially pediatric dentists, the new conventional GIs provide all of the advantages noted earlier in this article and result in better restorations than in times past. GIs should be considered for these clinical situations, especially for initial lesions in caries-active patients.
Liners—This is not a new use. 3M’s Vitrebond Plus, GC’s Fuji Lining LC, and other RMGIs have long been used as thin liners for restorations. Their partial light cure and ease of use have made this concept viable, and these materials have proven themselves over decades of use. Although the clinical need for liners is somewhat controversial in the scientific literature, the observational clinical success of liners in deep preparations is a testimony to the desensitization characteristic of such liners.
Bases—Liners are thin (approximately 0.5 mm), while bases are thicker (> 0.5 mm). A common question posed to CR from practitioners is why some tooth restorations with only a thin layer of bonding agent are sensitive. Although controversial for some practitioners, empirical evidence shows that thick bases in very deep preps with no pulp exposure usually have no postoperative tooth sensitivity. CR suggests application of a glutaraldehyde/HEMA solution for two one-minute applications before placing the conventional GI base. Examples are Kulzer’s Gluma and Zest Dental Solutions’ MicroPrime. The new, improved characteristics of conventional GIs make these materials ideal for bases. The absence of postoperative sensitivity is immediately evident to questioning practitioners. The research on the cariostatic effect of these materials is impressive.
Placement inside of tooth preps as a dentin replacement (sandwich technique)
Some dentists are using the new conventional GIs as complete dentin replacements. This concept is well proven and has been used for many years as theHere is a technique using GI inside and resin-based composite externally on a direct restoration (figure 5):
- Make a dry field.
- Prepare the majority of the prep first, leaving removal of the deepest caries portion until the last step in caries removal.
- Place glutaraldehyde-containing desensitizer/disinfectant for two one-minute applications (MicroPrime, G5, Glu/Sense, Gluma, or others with 5% glutaraldehyde and 35% HEMA). Don’t wash off; suction off instead.
- Place Equia Forte, Ketac Universal, or another brand of the new generation of GIs.
- Acid-etch the prep.
- Wash and dry.
- Place a bonding agent and cure.
- Place composite, cure, and finish.
Summary
GIs have really changed! They are much better than the previous generations of materials. Conventional GIs are the only dental materials to date that actually seal the tooth preparation, and they are one of the only dental materials that is cariostatic. This article discusses some of the unique uses for these new materials.
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on GIs for you and your staff.
One-hour videos:
- The NEW Glass Ionomers Really Work (Item V3514)
- Treating the Aging Population—A Frustrating Challenge (Item V4777)
Two-day virtual courses:
- Faster, Easier, Higher Quality Dentistry with Dr. Gordon Christensen. (One of our most popular courses, this will change your life, your production, and your revenue.) March 5–6, 2021.
- Restorative Dentistry 1—Restorative/Esthetic/Preventive with Dr. Gordon Christensen. March 26–27, 2021.
For more information about these educational products, call (800) 223-6569 or visit pccdental.com.
Gordon J. Christensen, DDS, PhD, MSD, is a practicing prosthodontist in Provo, Utah. He is the founder and CEO of Practical Clinical Courses, an international continuing education organization founded in 1981 for dental professionals. Dr. Christensen is cofounder (with his wife, Rella Christensen, PhD, RDH) and CEO of Clinicians Report.