Assisted periodontal therapy: a new dental hygiene paradigm
By Lynne H. Slim, RDH, MS, and Cynthia A. Chillock, RDH, EF, AP
For most folks, not a Christmas break goes by without their watching an interesting movie or DVD. For history buffs, a fascinating documentary series about the Tower of London is available for purchase in the U.S. It explores the history of this famous landmark and tourist attraction. The English are known for their love of tradition and attachment to the past, unlike their American counterparts. In one of this documentary’s eight episodes, a dignified gentleman who served as Constable of the Tower (most senior official) commented that tradition is the handrail that steadies us when the going gets rough. Tradition has its place in dentistry; however, dentistry needs to be receptive to new ideas and change is inevitable.
Some traditions in dentistry die hard, especially those theories/techniques/practice models that we learned from dental school professors. According to Dr. Paul H. Keyes, who spent several years as a senior researcher at the National Institute of Dental Research, many dentists thought that calculus caused periodontitis and, therefore, patients with more calculus had more disease. Back then, many oral health-care professionals didn’t even discuss periodontitis with patients unless the infection was advanced.
Dental hygienists were educated to focus specifically on calculus removal, and root planed for hours with newly designed Gracey curettes in an attempt to create glassy-smooth tooth and root surfaces. Dental floss, particularly the unwaxed variety, became the oral hygiene implement of choice in preventing the formation of unwanted calculus interdentally. The professional periodontal community adopted the specific plaque hypothesis in the 1980s and 1990s. This hypothesis implied that a few specific anaerobic microbes were associated with disease of the periodontium. Dental hygienists still worked in operatories, root planing teeth with Gracey curettes, but they – along with dentists – focused on educating patients on removing dental plaque and calculus.
Today’s dentists and dental hygienists have a different understanding of the etiology and progression of periodontitis. Periodontal researchers are forever bursting the theory “bubble.” We now understand that susceptibility to periodontitis is complex and multifactorial. We also know that periodontitis is an inflammatory disease caused by bacterial biofilms that accumulate on the teeth. Certain types of bacteria, and perhaps even herpes viruses, may trigger the disease. In many instances, this sets the stage for uncontrolled inflammation. Periodontal therapy, both nonsurgical and surgical, needs to be based on research evidence and clinical results.
Dental hygiene practice models in the first decade of the 21st century
Many dental hygiene practitioners now practice as periodontal therapists. They have three goals in mind: healthy patients, job satisfaction (happiness at work as a result of good teamwork), and increased production. Practitioners who work on a one-hour recare schedule in a single operatory with limited assistance are struggling in several respects and becoming increasingly frustrated because too much is expected in the one-hour appointment. An unrealistic, rushed appointment often results in inadequate therapeutic outcomes and disease-masking.
Let’s look at a typical adult recare appointment and break down the appointment according to necessary tasks. An RDH needs to clean and disinfect the treatment area between patients. If he or she complies with the OSHA-required 10 minutes of kill time for adequate infection control, about 50 minutes of appointment time remains.
Updating the patient’s medical history and taking blood pressure, plus a preprocedural mouth rinse, take at least five minutes. Taking necessary radiographs adds another 10 to 20 minutes to the mix. Periodontal probing and recording without an assistant may take as long as 20 minutes.
If the dental hygiene clinician performs both the intraoral and extraoral cancer exams, another five minutes is used up. Polishing is another five- to 10-minute procedure. Many hygienists today are polishing prior to instrumentation to remove stain and reduce instrumentation time. Writing notes to pass the “amnesia test,” as recommended by risk management experts, may take another five to 10 minutes.
According to the above calculations, hygienists are working for approximately 55 to 70 minutes with no patient education and instrumentation other than routine polishing. Instrumentation to remove oral biofilms supra- and subgingivally along with calculus deposits takes time and cannot be rushed. After debriding a pocket, what if a local delivery antimicrobial is needed to further suppress oral biofilms? How can a hygienist feel anything but frustration when trying to offer a thorough, high-quality professional service under these conditions?
Unfortunately, this model is the current reality for most dental hygiene clinicians today. When working under these tight conditions, something has to give. Consequently, appointment shortcuts often follow. Most of the time these shortcuts occur in the areas of instrumentation and patient education. These are two portions of our tradition that we do not want to change! The harsh reality is that RDHs have more to do in the typical one-hour adult recare appointment time than is considered realistic and appropriate. When hygienists feel rushed, mistakes are made. Often shortcuts are taken when it comes time to update medical histories, write notes, and document relevant information.
When dental hygienists are not given adequate time to foster relationships due to a rushed appointment, it’s next to impossible to convey an understanding of the disease process and get patients to take ownership of their disease. To encourage patients to become more actively engaged in preventing or arresting disease, hygienists have resorted to communicating while instrumenting. This talking and working simultaneously does not really allow for any true dialogue between the patient and clinician. It creates an atmosphere of preaching or monologue with no patient feedback.
Scientific studies have shown that passive listening leads to only a small percentage of retention. If patients do not understand and cannot be adequately engaged in dialogue, their eyes gloss over and you will lose them. As a result, they are treated by “cookie cutter” techniques that do not allow for shared decision-making. If this is the only way a hygienist is communicating with patients, perhaps the hygienist should give patients written material to read on their own time. Without shared decision-making, patients will not understand the seriousness of their condition, and their beliefs and values will not be revealed.
Periodontal diseases now are being increasingly linked to systemic diseases such as rheumatoid arthritis, diabetes, and cardiovascular and pulmonary diseases. Research here is ongoing but inconclusive. Even so, it’s imperative to a patient’s total health that he or she understands the disease process and the inflammatory nature of periodontal diseases.
Chronic periodontitis is mostly a disease of middle age, with the majority of patients presenting in their 40s and 50s. Mild to moderate chronic periodontitis is the most common periodontal disease. It is estimated that approximately 40 percent to 60 percent of adults in the westernized world are affected. As the huge baby boomer population continues to age, the incidence of certain systemic diseases will undoubtedly influence the extent of periodontal disease experienced in the Western world.
Four-handed conservative periodontal care
By using a hygiene team that incorporates four-handed clinical periodontal care, patient participation will be enhanced in several ways. Reading periodontal data numbers out loud while an assistant is recording allows the patient to participate in an active listening exercise. This exercise will elicit questions of concern from the patient if the numbers are not within a normal range.
A patient who asks a question is a captive audience, ready to hear the answer. We call this a “teachable moment.” The assistant can calculate the data in a Periodontal Health Index and present a score to the patient. This is similar to using blood pressure numbers as a way to monitor health. By adding a patient’s pockets and bleeding points together, you arrive with a two-number total of pockets and bleeding points. (If you are still using paper charts, you can find them at www.perio-data.com.)
It is an easy way to monitor a patient’s periodontal health. With assistance, it’s also easy to assess a patient for oral cancer, dental caries, and periodontal risk by using PreViser analytic software (www.previser.com). PreViser scores create a baseline measurement of risk and disease from which future interventions can be more effectively planned and measured.
Oral health-care professionals are better prepared to handle acute illnesses. Chronic care models for managing oral diseases with a more proactive, organized approach are not yet the norm. Just as physicians and nurses monitor blood pressure and cholesterol readings, the PreViser analytical software and periodontal indices can be used to empower patients to take greater responsibility for their oral health. Patients will better understand referral to the periodontist, when data is tracked and a decision-support tool is used.
From a clinical perspective, hygienists have a better understanding of the role of oral biofilms and periodontal pathogens in the initiation of chronic inflammatory periodontal diseases. Research supports the use of power scalers to disorganize bacterial biofilms and suppress periodontal pathogens. When the assistant uses a high-volume evacuator during power scaling, there are fewer airborne pathogens released into the operatory. This results in better infection control and less cross-contamination.
When the hygienist is treating patients with hand instrumentation, the assistant can use a surgical suction tip where it is needed. No matter how good a hygienist is, no one can see through blood. Having a clearer field of vision when scaling and root planing periodontal patients makes a significant difference. If it can’t be seen, it can’t be removed.
By using indirect vision with the help of an assistant, clinicians can work in a more comfortable position. When seated in a compromised position for a long period, it’s difficult – if not impossible – to stay in that position long enough to complete necessary instrumentation. Greater physical comfort frees the body to spend time debriding the biofilms.
Effectiveness of instrumentation is a high priority for clinical excellence. The only way to measure success is by monitoring a patient’s periodontal health. If the patient heals, instrumentation was effective, and vice versa. It then becomes imperative that the hygienist determine the reason(s) for ineffectiveness. Does the patient have an autoimmune disease causing impaired wound healing? Does the patient need to come in more frequently for periodontal maintenance? Does the patient need to work harder to control oral biofilms at home? Did the hygienist have time to customize and demonstrate an appropriate home-care regimen? Did he or she leave residual calculus and/or biofilms behind because of a lack of time, dull instruments, or the hygienist was working blind?
Patients who understand their disease and/or periodontal health status become more involved in their care. By establishing optimum oral health, patients have a better appreciation for partial- or full-mouth restoration when it becomes necessary and will appreciate the healthy foundation for restorative enhancements. Appointments and clinical care based on each patient’s needs are the hallmark of clinical excellence. A clinician’s frustration level is greatly reduced when adequate time is given for conservative periodontal therapy. Most important, when hygienists share a patient’s time requirements with an assistant, it frees up the clinician’s time to address each patient’s needs and customize an optimal care plan. Successful treatment for patients makes for happy team members, and happy team members make patients happy. Satisfied, involved patients follow through with other dental care. Their adherence to a comprehensive treatment plan will ensure a better bottom-line number for the practice.
When we treat everyone the same with a one-hour appointment, no matter what he or she needs, boredom and frustration enter the dental practice. It is impossible to do your best work if you are bored or frustrated with your career, and to give your all to the task at hand if you are in painful, compromising positions and cannot see. It is easy to feel “burned out.” For these reasons, many great clinicians leave dental hygiene.
An effective alternative to dental hygiene burnout is four-handed conservative periodontal therapy. The assistant can seat patients, update medical histories, take radiographs, record periodontal data, suction throughout entire appointments (this may include localized antimicrobial placement), and write most of the treatment notes.
At the end of the appointment, the hygienist can customize home-care education and post-treatment instructions while the assistant moves on to the next patient. The RDH can take the necessary time to make sure the patient understands the disease process and what kind of treatment is required to restore health. At the end of the day, patients and clinicians are less frustrated, and clinicians discover the care they delivered was more successful and profitable.
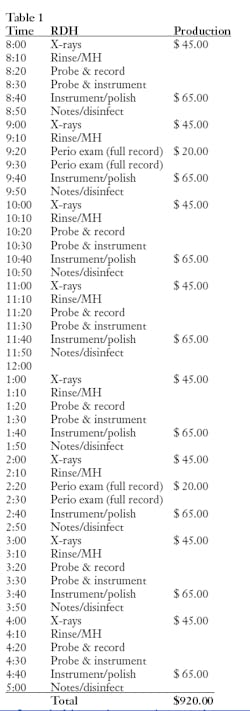
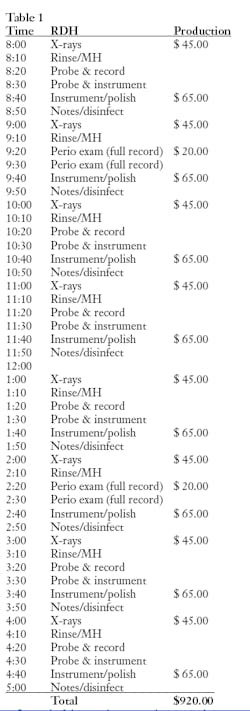
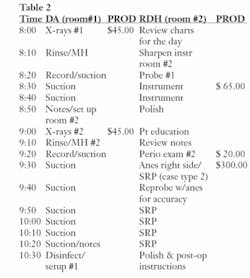
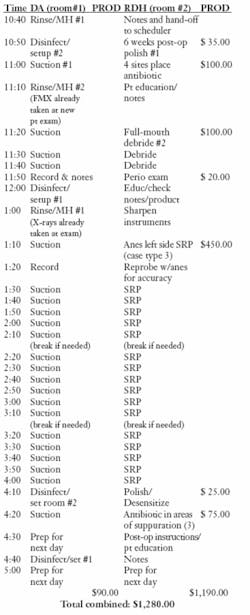
Let’s take a look at a traditional one-operatory hygiene daily schedule, and then compare it to four-handed clinical care (see Tables 1 and 2).
Instead of the one-hour appointment where everyone is treated the same, including radiographs (Table 1), hygiene appointments now have much more flexibility and look something like this:
DA cleans and disinfects the treatment area between patients, requiring 10 minutes kill time for adequate infection control. Updating the medical history and taking blood pressure plus preprocedural rinse takes about five minutes. Processing radiographs requires 10 to 20 minutes. Probing and recording with an assistant takes 10 minutes instead of 20. An intraoral and extraoral cancer exam requires five minutes and polishing takes about five minutes. The majority of notes are written by the assistant and may require another five minutes for the hygienist to check for accuracy and make necessary additions.
This requires 25 minutes of time with the assistant up front, and 20 minutes of assistant and hygienist time for probing and polishing. So far, the RDH has used only 20 minutes of the appointed hour time slot. If there is still a need to leave 10 minutes of education and note checking at the end of the appointment, this leaves 30 minutes of instrumentation time.
When the duties are shared with a dental assistant, instrumentation time will increase from five to 15 minutes per patient to about 30 to 35 minutes. Your hygienist can’t help being more clinically successful, and this is just on healthy maintenance cases.
If each patient’s care is individualized to allow enough time for thorough instrumentation, more advanced conservative periodontal cases become more workable on the appointment schedule (Table 2).
Not having to turn the rooms around every hour and do all the updates can free a dental hygienist to have more time for instrumentation. By doubling appointment times, actual instrumentation time is increased so that the clinician can thoroughly debride biofilms from the root surfaces. This provides for greater therapeutic success in these cases.
In Table 2, it’s obvious the assistant’s salary is more than compensated for by the day’s increased hygiene production. In this example, the increase was $360.This total does not include any fee for products that may be dispensed.
Getting back to old traditions, it’s important to keep in mind that change and modification of tradition become necessary when new models and theories replace outdated ones. If clinicians continue to practice high-quality, compassionate care that includes evidence-based decision-making, patients will arrive at a practice’s front door asking, “What’s new?” instead of expecting the same old tired routine with familiar but outdated procedures.
Editor’s note: References available upon request.
Cynthia A. Chillock, RDH, EF, AP, is a consultant, speaker, author, advanced instrumentation and four-handed clinical care trainer, CEO of Perio-Data™, as well as creator and lead singer for the Salivary Singers. Chillock is a member of the DANB-Infection Control Exam committee. Her career has spanned more than 42 years with the last 27 limited to conservative periodontal therapy. Reach Chillock by phone at (520) 323-5602 or by visiting the Web at www.perio-data.com or www.salivarysingers.com.
Lynne Slim, RDH, MS, perio therapy columnist for RDH magazine, is an award-winning dental author who has published extensively in dental and dental hygiene journals. Slim is the CEO of Perio C Dent, a dental practice management company that specializes in the incorporation of conservative periodontal therapy into the hygiene department of the general dental practice. Slim coaches dental hygienists and dentists in ultrasonic instrumentation and other advanced hygiene initiatives. Contact her at [email protected] or www.periocdent.com.