With all the latest talk about COVID-19 and its ramifications across the spectrum of all that’s health care, it’s no surprise that the manifestations of this virus creep over into oral health care and what we as dentists are subsequently managing. Pathology is no exception.
Let’s assess two pathology cases I’ve seen and diagnosed on multiple levels and on numerous occasions in my practice, both of which are directly correlated with COVID-19.
Case no. 1
A generally healthy, spry-as-they-get, 94-years-young female presents for her recall exam with the chief complaint of a “burning mouth with white patches under my front lip.” Duration had been approximately three weeks. Medications were for thyroid issues and long-term breast cancer (tamoxifen).
Clinical evaluation revealed scattered, white, creamy patches in the lower anterior vestibule, each measuring approximately 3–6 mm (figure 1). Now, take a look at the second picture after the white patches were easily wiped off with gauze (figure 2). Note the red, thin-membraned tissue? It was very tender to the touch and sensitive even to air.
This diagnosis should be a slam dunk—pseudomembranous candidiasis, aka thrush. Let’s have a refresher.
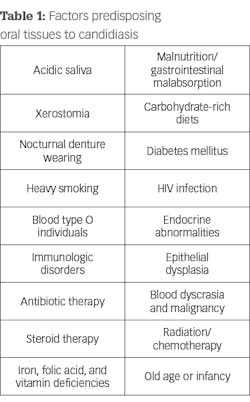
Candida albicans presents as commensals that become infective when an alteration in the immunity of the host occurs; it’s opportunistic and usually the first to take advantage of any reduction in the defense system of the host cell. Oral imbalances are common and a frequent place for these infections to occur.1 Oral clinical appearances vary—some present as white patches/lesions (some rub off, others don’t), while others appear bright red in color. See Table 1 for a list of predisposing factors for candidiasis.
- Acute pseudomembranous candidiasis consists of creamy, loose patches of desquamative epithelium that are easily removed.1 Red tissue tender to the touch is what is painful to the patient.
- Atrophic (erythematous) candidiasis presents with bright red, thinned and smooth mucosa with burning and sensitivity. It is commonly referred to as “denture sore mouth.”1
- Chronic hyperplastic candidiasis consists of white plaques or papules against an erythematous background. It is asymptomatic and does not rub off.1 A case presented in DE’s Through the Loupes newsletter, “Oral pathology case: A brush with thrush . . . or is it?” was diagnosed to be this form of thrush.
With all C. albicans infections, treatment is nystatin (as a rinse or swab), clotrimazole (commonly prescribed as a troche/lozenge), and Diflucan/fluconazole (commonly prescribed as an oral medication). Magic mouthwash, in cases where pain in present, helps manage the symptoms until the lesions heal. (Recipe: one part viscous 2% lidocaine, one part Maalox, and one part diphenhydramine 12.5 mg/5 ml. Dosage: 1–2 tsp. 2–3x/day prn. I usually give 1–2 refills with a 150 ml bottle.)
Troche lozenges and Magic mouthwash were prescribed along with ways to reduce stress and relax. Follow-up 10 days later was positive with a significant reduction in signs/symptoms.
Case no. 2
A 62-year-old male presents with the chief complaint of a “large sore on the roof of my mouth.” The patient was from out of town and had called his oral surgeon in San Diego with an inquiry as to what he should do. The doctor called in a script of amoxicillin 500 (“just in case it was bacterial”) with further instructions to seek a clinical assessment with a dentist should the lesion not improve.
After five days, there were no changes. The patient shared that the lesion and area in general were very sensitive to acidic foods and painful overall when eating and functioning with day-to-day activities. He reported significant stress with his job due to travel/COVID-19 and the impact of things beyond his control.
The clinical exam revealed a large 12x9 mm lesion on the left side near the junction of the hard and soft palate. It was creamy white in color with irregular erythematous borders, most notably advanced in the oropharyngeal direction (figure 3).
Differentials include trauma, aphthous major, autoimmune disorders, and viral and nutritional deficiencies.
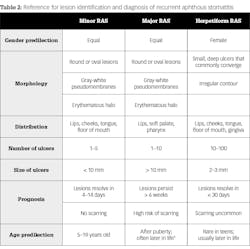
Definitive diagnosis is aphthous major, the second most common form of recurrent aphthous stomatitis (RAS). RAS, also commonly known as a canker sore, is the most common condition of the mucosal soft tissue in the oral cavity, affecting 15%–20% of the world’s population.1 These conditions take on three different clinical forms: aphthous minor, aphthous major, and herpetiform ulcers. See Table 2 for a go-to reference for these three lesions.2
Causes
Most patients who are diagnosed with RAS are healthy; however, there are those with systemic conditions or compromised immune systems who are more prone to having RAS, specifically those with Behcet’s syndrome and chronic gastrointestinal malabsorption disturbances (Crohn’s and celiac diseases), which create nutritional deficiencies of folic acid, vitamin B12, and iron.1
Furthermore, correlation has been found with the menstrual cycle, periods of stress and anxiety, and family history.1 In this particular case, the patient reported being under severe stress of late due to recent COVID-19 pandemic concerns with work and outside influences.
Treatment
It is advisable that the underlying cause of the issue be treated initially. With this case and others of a similar nature, it is recommended that the patient alleviate stress and systemic compromises. There is no doubt that the recent pandemic and the anxieties that have been placed on society have had a trickle-down effect on the general health, well-being, and mental stability of numerous individuals.
In addition to assessing the underlying contributing cause, treatment is otherwise supportive and palliative with topical and systemic medicinal application modalities. Topical treatment is beneficial in preventing superinfections and decreasing infections and the subsequent potential for secondary bacterial infections.2
Chlorhexidine 0.2% rinse helps eliminate gram-positive and -negative bacteria and fungi and prevents the buildup of biofilms.2
A prescription for Magic mouthwash was given, and follow-up a couple weeks later proved to be positive. The patient furthermore reported significantly reduced stress levels.
Editor’s note: Adapted from Through the Loupes pathology cases. Through the Loupes is a publication of the Endeavor Business Media Dental Group. Read more articles at dentistryiq.com/dentistry and subscribe at dentistryiq.com/subscribe.
References
- Sapp JP, Eversole LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology. Mosby; 1997:4-5,245-249.
- Edgar NR, Saleh D, Miller RA. Recurrent aphthous stomatitis: a review. J Clin Aesthet Dermatol. 2017;10(3): 26-36.