Editor's note: First published in 2016; reviewed for clinical accuracy in 2022.
Q: Over the last few years I have placed many full-zirconia crowns and a few zirconia three-unit bridges. Overall, I have been pleased with the clinical results. The only objectionable esthetic quality is that most of the restorations I receive back from the lab appear to have a lighter color than I requested. This is a relatively minor problem, since most of them are in the posterior area of the mouth where an outstanding esthetic result is not mandatory. The significant challenge I am having, however, is that far more zirconia restorations come off during service than I ever had with porcelain-fused-to-metal restorations in the past. What can I do to eliminate this disagreeable, time-consuming situation that is also frustrating to patients?
A: Full-zirconia restorations have been available for the past years or so. They have evolved from relatively unesthetic, opaque crowns and bridges to significantly improved restorations with acceptable esthetics (figures 1 and 2). Most dentists have noted that the majority of zirconia restorations are lighter in color than they requested on their lab order. The intense opacity of this material makes the restorations appear light in color. As the new generation of "esthetic zirconia" restorations continues to improve, this color problem will probably be overcome.
In the meantime, I suggest that you take photographs of the tooth or teeth to be restored. Place the shade guide color tab directly adjacent to the tooth or teeth you are restoring. Don't print the image. Color printing often distorts the color, because the inks used in printers vary significantly. E-mail these images to your lab. When you send the color electronically, it is usually close to the actual requested color. Along with these photographs, ask the laboratory technician to make the restoration color as close as possible to the color of the shade guide shown in your picture.
Figure 1: These full-zirconia fixed prostheses have served in the mouth for three years. Clinicians Report Foundation has research (TRAC Division) on zirconia-based three-unit fixed prostheses now serving for nearly 12 years.
Figure 2: Full-zirconia restorations on the first and second molars show the significant improvement in color now available with full-zirconia restorations.
If the technician has an actual photo to copy, the likelihood of your receiving the correct color is much improved. If you are not successful in doing this, request a color one shade darker than you actually need. We have found that the color of the blocks from which some of the zirconia crowns are milled actually vary from one another even though they have the same color designation printed on their packaging. I feel confident that this challenge will be overcome as these restorations continue to grow in popularity.
Related reading:
Improving the color match of zirconia crowns
Zirconia crowns coming off while in service
This is not just your problem. In many of my seminars, I hear dentists complain about zirconia restorations frequently coming off. Our science team at Clinicians Report Foundation (CR) has studied this problem in depth, and we have some of the answers. However, the team is still studying various aspects of the problem.
At this time, we see several potential reasons why some zirconia restorations come off during service:
• Avoid any contact of phosphoric acid with the zirconia restoration during the cementation process. The phosphate ion in the acid greatly reduces any potential bonding to the zirconia.
• Do not clean the tooth preparations with prophy paste. The emollients and fluoride in some prophy pastes can be negative and cause crowns to come off. Use flour of pumice and water. A good example product for this is Preppies from Whip Mix (figure 3).
• Use resin-modified glass ionomer (RMGI) cement for zirconia restorations when the tooth preparations have near-optimum characteristics. See Figures 4 through 6 for examples of these characteristics. Most clinicians and researchers would agree that the tooth preparation should be at least 4 mm in height from the gingival margin to the occlusal table, and that the lack of parallelism of the preparation walls should be up to, but not more than, 20 degrees from the long axis of the tooth being prepared.
• We are currently researching whether or not we need to place a bonding agent on the tooth surface to potentially enhance the bond of the resin component of the RMGI cement (20% resin) to the tooth. The CR study (by CR's TRAC research division), now going into 12 years in the mouth, cemented zirconia-based three-unit fixed prostheses to preparations with RMGI without any bonding agent on the tooth preps. There has been only 4% debonding of the prostheses over that period of time. We conclude from that in vivo study that a bonding agent is not needed. However, the ongoing research currently under way in CR soon will answer that question more thoroughly.
Figure 3: Use of materials for cleaning tooth preparations such as Whip Mix Preppies eliminates some of the contamination when using prophy paste.
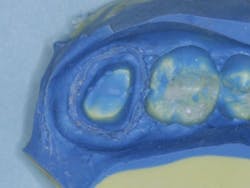
Figures 4-6: Images showing an adequate impression, the die of an adequate tooth preparation, and the resultant full-zirconia crowns.
Figure 4
Figure 5
Figure 6
• The same study noted above did not place zirconia primer on the internal of the zirconia restorations when the RMGI cement was used. Currently we are studying that aspect of the cementation process to see if the zirconia primer will enhance the bond of RMGI to the zirconia surface. Empirical evidence from this study indicates that the zirconia primer is not needed when RMGI cement is used. However, zirconia primer still appears to be indicated when resin cement is used.
Cementing zirconia restorations with RMGI
At the time of this publication, it appears that the cementation procedure for zirconia restorations over preparations with the desirable characteristics described above is adequately accomplished with RMGI cement (figure 7).
Figure 7: RMGI is the recommended cement for full-zirconia restorations. Two of the most popular RMGI cements are shown.
Tooth preparations with minimal retention
What about tooth preparations that do not have 4 mm of axial walls and are tapered more than 20 degrees from the long axis of the tooth preparations?
For these clinical situations, many dentists have elected to use the self-adhesive resin cements (bonding materials are incorporated in the cement) or adhesive cements (bonding material is placed on the tooth preparation prior to cementation). Respective example brand names are RelyX Unicem 2 (3M ESPE) or Maxcem Elite (Kerr Dental) for self-adhesive cements, and Multilink Automix (Ivoclar Vivadent) or Panavia (Kuraray Dental) for the adhesive cements.
However, CR's TRAC research division has shown more debonding of zirconia restorations cemented with these resin cements than those cemented with RMGI cements, despite their being stronger than RMGI cements. To reduce the debonding problem with resin cements, CR research1 has shown that placement of a bonding agent on the tooth preparation and on the internal side of the zirconia restoration before cementing with self-adhesive or adhesive cements significantly increases their bond to tooth structure. The unfortunate situation relative to cementing procedures for zirconia restorations is that there is no agreement among manufacturers of cements as to the best technique.
At the time of this writing, the conclusions based on research by the CR Foundation science and clinical teams are as follows:
• Retentive prep: Sandblast the internal of the zirconia restoration or clean it with Ivoclean (Ivoclar Vivadent). Clean the tooth preparation with flour of pumice and water on a rubber cup, place a desensitizer/disinfectant on the tooth preparation for two one- minute applications (examples are Gluma from Heraeus Kulzer or MicroPrime from Danville Materials) and suck it off (don't wash it off), and then seat with RMGI cement.
• Minimally retentive prep: Sandblast the internal of the zirconia restoration or clean it with Ivoclean. Place an MDP primer on the internal of the restoration (e.g., Z-Prime Plus from Bisco Inc., Monobond Plus from Ivoclar Vivadent). Roughen the tooth preparation with a coarse diamond and clean the tooth preparation with flour of pumice and water on a rubber cup. Place a tooth desensitizer/disinfectant on the tooth preparation and suck it off (don't wash it off). Place a bonding agent on the internal of the restoration and on the external of the tooth preparation, then seat with a self-adhesive or adhesive cement as identified previously.
Summary
It is apparent that full-zirconia restorations are working well and that they are now the most commonly used posterior tooth indirect restorations used in the United States. They are also significantly improving in color. However, restorations coming off during service continue to be a clinical challenge. The techniques in this article have been researched by Clinicians Report Foundation and are state of the art in cementation of zirconia restorations. However, ongoing research on some lingering questions may change the suggestions in the future. Watch for such changes as this research is completed.
Reference
1. Christensen GJ. Self-Adhesive Resin Cements: Are They Working? CR Clinicians Report. 2015;8(5).