Albert Yoo, DDS
Root-form endosseous implants have long been touted as the ideal option for "permanent" tooth replacement, with success ranging from 96% to 98%. Implant dentistry has exploded in practice and revolutionized our profession. For a while, "premier" implant companies held the largest market share, offering their implants and components at premium prices. But, as in all burgeoning industries, there came a rapid influx of competition. Many companies-branded as knock-off or lower-tier companies-began offering inferior quality products but at significant monetary savings.
But can these economical implants provide integrated, stable, functional, and esthetic restorations? What are the science and economics behind a $100 implant? In other words, is there a difference between a $100 dental implant and a $400 one? (The short answer is: $300.)
| Table 1: Implant tier system | |
Tier 1 | Research supports the long-term use and success of implant systems in this category. These systems are regarded with the highest perception of quality and are available at premium costs. |
Tier 2 | Scientific studies support the success of these implant systems, which have moderately priced components. |
Tier 3 | Little or no research supports the clinical application of implant systems in this tier, which includes the least reputable "clone" implants, often available at the lowest costs. |
The implant tier system is based on perceived brand recognition, reputation, and cost (table 1). Many would consider only Tier 1 implant fixtures because of clinical research and time-tested reliability. Tier 2 implants may also have scientific studies supporting their efficacy, but they may also be more economically priced. Tier 3 implants are considered to be less reputable "clone" implants, with little or no research supporting their longevity as well as reports of poor-fitting components.
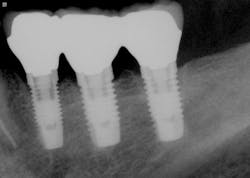
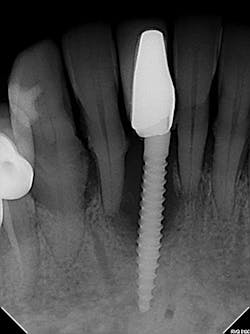
The most critical aspect of any implant system is the interface between the implant fixture and its surrounding bone (figures 1-5). Integration between the fixture and its surrounding bone is the foundation of modern implant dentistry. There is little we can do to modulate bone healing, but we can modify the implant fixture itself.
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Figures 1-5: Figures 1 through 4 illustrate, respectively, a seven-year follow-up visit and a three-year follow-up visit of two different implant systems. Implant No. 22 (figure 5) shows peri-implant radiolucency following functional loading, indicating fibroencapsulation and loss of integration into bone, necessitating removal.
Implant characteristics
Titanium
Modern implant fixtures are fabricated with titanium. Titanium is used because of its osseointegrative properties, discovered first by Per-Ingvar Brånemark. All endosseous dental implants currently manufactured and surgically placed are made of titanium metal, whether commercially pure or an alloy. All implants manufactured from titanium will integrate into bone with varying degrees of bone-implant contact (BIC). How much BIC is actually necessary for long-term implant stability is unknown, and instruments to measure stability are inadequate in providing correlation with BIC.1 Different implant companies, however, attempt to distinguish their products primarily by varying surface treatment and implant design.
Surface treatment and microgeometry
The original Brånemark implant was a turned or machined smooth surface. This implant integrated well, following a healing period of up to six months post-placement. Advances in technology have mostly come in the form of surface treatment; roughened and treated implant surfaces expedited the integration process, allowing faster bone-implant contact with shorter waiting periods to final restoration. Promising faster, stronger, and more stable integration, manufacturers use different processes to treat or coat their implant fixtures, including: acid-etching, blasting and acid-washing or -etching, hydroxylapatite-coating (HA-coating), laser ablation, plasma-spraying, etc.2 Although some practitioners believe that certain manufacturers' implant surface treatments are superior to others', research has shown that implants with all of the aforementioned surface treatments can successfully integrate, with no surface providing any benefit over another.2-6 Several studies have been performed that cast one implant company over another, with no statistical difference in implant failure rate.7-10
Implant design and macrogeometry
Studies have shown increased implant success with higher initial insertion torque. Companies have continuously evolved implant design in terms of taper, thread depth and pitch, and spiral bone channels. In search of better crestal bone preservation and soft-tissue stability, numerous implant collar modifications have been offered, including: micro threads, platform switch, and internal or conical connection. No studies indicate whether one implant design is superior to another,11 as multiple variables determine implant success.
Implant fixture design continues to evolve to aid surgeons in achieving primary stability in soft bone, less-available bone, and/or for purposes of immediate load (figure 6). While one design is not superior to any other in success, each design has its surgical and restorative application.
Tolerance and fit of implant components
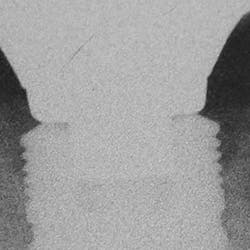
Implant manufacturing involves a high degree of precision. Implant fixture dimension, bone drill protocols, taps, and insertion devices should intimately correspond. Prosthetic components, abutment connections, and screws are also closely mated in design and production, so there is minimal tolerance between machined components. Interestingly, I hear much conversation regarding the poor fit of lower-tiered implant components, which can result in implant failure or screw loosening. Implant systems consist of CAD/CAM parts, with components that are fabricated with a high degree of homogeneity. Vertical and anti-rotational discrepancies exist and vary between companies and the types of connection used,12 but studies indicate that the fit of mismatched components improves with the application of mechanical torque to a clinically acceptable level.13 Clinicians also need to understand that there is more to screw loosening than the system-such as passive fit of the casting, proper torque values and preload,14 adequate interproximal contact, and the most often overlooked and misunderstood aspect of dentistry . . . occlusion (figures 7-9).
Figure 6: Various implant fixture designs
Figure 7
Figure 8
Figure 9
Figures 7-9: Implant site No. 19 has been restored for one year without any incident of screw loosening. Bone levels are excellent (figure 7), but a small gap is evident between the abutment and fixture platform upon radiographic evaluation (figure 8), due to the usage of implants from two "compatible" manufacturers. The tissue levels are excellent, despite a "mismatch" in components. Notice the gingival recession and the lack of attached tissue15,16 on distal implant site No. 18 (figure 9). However, with critical examination of implant No. 18, it is possible that the transmucosal element is too long and the overlying gingival tissues too thin, making this particular fixture inappropriate for this site. (Perhaps a bone-level fixture would have been a better choice.)
| Table 2: Factors influencing implant failure and success17 | |
Medical history | Smoking,18 diabetes,5 penicillin allergy,19 patient variability |
Status of dentition | Periodontal, endodontic |
Bone | Volume, type, jaw, region |
Tissue | Biotype, attached gingiva15,16 |
Surgical techniques | Preoperative antibiotics,20 drill sequence/protocols,21,22 3-D placement, initial stability,23,24 grafting procedures, clinician experience25,26 |
Integration | Latency period, immediate load,10 denture |
Prosthetics | Cement, occlusion, design |
Maintenance protocols27 | Frequency, patient hygiene |
| Table 3: The economics: Tier 1 implants versus Tier 3 implants | |||||||
Fixture | Cover screw | Healing abutment | Impression coping | Lab analogue | Castable abutment | Case total | |
Tier 1 | $400 | $25 | $55 | $100 | $100 | $200 | $880 |
Tier 3 | $175 | Included | $20 | Included | $35 | $100 | $330 |
Difference: | $550 | ||||||
Savings at 100 implants per year | $550 x 100 = $55,000 | ||||||
Surgical savings: $285 x 100 = $28,500 | Restorative savings: $265 x 100 = $26,500 | ||||||
Implant failure is not solely a result of the system used but rather the result of a diverse range of factors, which can include: the patient's medical and dental histories, as well as the employed surgical, prosthetic, loading, and maintenance protocols (table 2; figures 10-20). Despite the dental community's poor perception of lower-tier and more economical implants and the marketing of premium-priced systems, scientific evidence and good clinical judgment support their validity in clinical application. Renowned implant pioneer and professor George Zarb has said, "Implants don't fail. When implants are appropriately placed in healthy patients, they achieve osseointegration. If implants fail, it is due to operator error."
The question is not, "Which implant system is the best?" but rather, "Which implant system is appropriate for the particular surgical and restorative scenario, while remaining cost-effective for the dental practice?" One cannot simply ignore the economics (table 3) behind the $100 implant. And as dental practitioners, we should never equate cost to a successful treatment outcome!
Figures 10-11: Implant failure can occur as a result of the periodontal and/or endodontic status of the adjacent teeth.
Figure 12: The implant position in this photo is placed too far facially, compromising the buccal bone. This implant, if not removed, will fail because of surgical error.25,26
Figures 13-16: This implant was immediately placed and loaded by a foreign dentist. The entire assembly was mobile upon clinical presentation. This implant failed because it was immediately loaded without attention to the patient's occlusion and not necessarily due to implant position, improper abutment seating, or poor contours of the temporary restoration.
Figure 13
Figure 14
Figure 15
Figure 16
Figure 17: A severe cupping defect was noted radiographically for implant No. 31, believed to be due to occlusal forces (terminal molar).
Figures 18-19: The patient presented with two failing implants (≥50%). Before ascertaining the implant system used, several factors need to be considered: the patient's history of smoking,18 the extraction and grafting procedures performed, the patient's untreated periodontal disease and oral hygiene,27 the 3-D implant position, the prosthetic design (including open contact) and occlusion, and the lack of attached gingival tissue.6,15
Figure 18
Figure 19
Figure 20: Excess cement was noted on evaluation of the implant, along with the periapical radiolucency of No. 29. Despite our best efforts to remove this cement and verify radiographically, proper and complete removal will necessitate surgical entry to prevent bone loss from "peri-cementitis."
References
1. Manresa C, Bosch M, Echeverria JJ. The comparison between implant stability quotient and bone-implant contact revisited: an experiment in Beagle dog. Clin Oral Implants Res. 2014 Nov;25(11):1213-21.
2. Abrahamsson I, Berglundh T. Effects of different implant surfaces and designs on marginal bone-level alterations: a review. Clin Oral Implants Res. 2009 Sep;20 Suppl 4:207-15.
3. Bullis G, Shah S. Implant surface treatments: a literature review. Inclusive Magazine 5;2:87-89.
4. Glauser R, Rée A, Lundgren A, Gottlow J, Hämmerle CH, Schärer P. Immediate occlusal loading of Brånemark implants applied in various jawbone regions: a prospective, 1-year clinical study. Clin Implant Dent Relat Res. 2001;3:204-213.
5. Morris HF, Ochi S, Winkler S. Implant survival in patients with type 2 diabetes: placement to 36 months. Ann Periodontol. 2000 Dec;5(1):157-165.
6. Palmquist A, Omar OM, Esposito M, Lausmaa J, Thomsen P. Titanium oral implants: surface characteristics, interface biology and clinical outcome. J R Soc Interface. 2010 Oct; 6(7) Suppl 5:S515-27.
7. Astrand P, Engquist B, Dahlgren S, Grondahl K, Engquist E, Feldmann H. Astra Tech and Branemark system implants: a 5-year prospective study of marginal bone reactions. Clin Oral Implants Res. 2004:15:413-420.
8. Batenburg RHK, Meijer HJA, Raghoebar GM, van Oort RP, Boering G. Mandibular overdentures supported by two Branemark, IMZ or ITI implants. A prospective, comparative preliminary study: one-year results. Clin Oral Implants Res. 1998;9:374-383.
9. Geertman ME, Boerrigter EM, Van Waas MA, van Oort RP. Clinical aspects of a multicenter clinical trial of implant-retained mandibular overdentures in patients with severely resorbed mandibles. J Prosthet Dent. 1996;75:194-204.
10. Gelman AS, Verban EM. Long term clinical survival of two tissue level implant systems with different surface modifications: a retrospective comparison with up to five-year results. J Implant and Adv Clin Dent. 2011 May/June; 3(4):29-35.
11. Esposito M, Coulthard P, Thomsen P, Worthington HV. The role of implant surface modifications, shape and material on the success of osseointegrated dental implants. A Cochrane systematic review. Eur J Prosthodont Restor Dent. 2005 Mar;13(1):15-31.
12. Binon PP. Evaluation of machining accuracy and consistency of selected implants, standard abutments, and laboratory analogs. Int J Prosthodont 1995;8:162-178.
13. Solá-Ruíz MF, Selva-Otaolaurruchi E, et al. Accuracy combining different brands of implants and abutments. Med Oral Patol Oral Cir Bucal. 2013 Mar 1;18(2)e332-6.
14. Kim KS, Lim YJ, Kim MJ, Kwon HB, et al. Variation in the total lengths of abutment/implant assemblies generated with a function of applied tightening torque in external and internal implant-abutment connection. Clin Oral Impl Res. 2011;22:834-839.
15. Kim BS, Kim YK, Yun PY, et al. Evaluation of peri-implant tissue response according to the presence of keratinized mucosa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(3):e34-e38.
16. Yoo A, Bear A. (2014, May 6). Attached gingiva and dental implants. [Web blog post] Retrieved from: http://www.surgicalrestorative.com/articles/2014/05/attached-gingiva-and-dental-implants.html.
17. Chrcanovic BR, Albrektsson T, Wennerberg A. Reasons for failures of oral implants. J Oral Rehabil. 2014;41:443-476.
18. Lambert PM, Morris HF, Ochi S. The influence of smoking on 3-year clinical success of osseointegrated dental implants. Ann Periodontol. 2000;5:79-89.
19. Wagenberg B, Froum SJ. A retrospective study of 1,925 consecutively placed immediate implants from 1988 to 2004. Int J Oral Maxillofac Implants 2006;21:71-80.
20. Dent CD, Olson JW, Farish SE, Bellome J, Casino AJ, Morris HF, et al. The influence of preoperative antibiotics on success of endosseous implants up to and including stage II surgery: a study of 2,641 implants. J Oral Maxillofac Surg. 1997;55:19-24.
21. Albrektsson T, Gottlow J, Meirelles I, Ostman PO, Rocci A, Sennerby L. Survival of NobelDirect implants: an analysis of 550 consecutively placed implants at 18 different clinical centers. Clin Implant Dent Relat Res. 2007;9:65-70.
22. Sennerby L, Rocci A, Becker W, Jonsson L, Johansson LA, Albrektsson T. Short-term clinical results of Nobel Direct implants: a retrospective multicentre analysis. Clin Oral Implants Res. 2008;19:219-226.
23. Morris HF, Ochi S, Orenstein IH, Petrazzuolo V. AICRG, Part V: factors influencing implant stability at placement and their influence on survival of Ankylos implants. J Oral Implantol. 2004;30:162-170.
24. Ottoni JM, Oliveira ZF, Mansini R, Cabral AM. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants 2005;20:769-776.
25. Albrektsson T. Is surgical skill more important for clinical success than changes in implant hardware? Clin Implant Dent Relat Res. 2001;3:174-175.
26. Lambert P, Morris HF, Shigeru O. Positive effect of surgical experience with implants on second-stage implant survival. J Oral Maxillofac Surg. 1997;55:12-18.
Albert Yoo, DDS, completed his predoctoral training at the Stony Brook School of Dental Medicine in 2005. He received his certificate in periodontics and implantology in Stony Brook in 2008. He is in full-time private practice and has lectured to numerous study clubs, with special interest in perio-prosthetics, advanced bone grafting, sinus lift procedures, and immediate implant placement. He is a clinical assistant professor in the Department of Periodontics at Newark Beth Israel Hospital, Stony Brook School of Dental Medicine, and New York Hospital of Queens. He maintains a private practice in Bayside, New York.