Louis Malcmacher, DDS, MAGD
One of the most common causes of bruxism will surprise many of you reading this article. Here's a hint: It's related to sleep.
Let's look at some facts: Dental sleep medicine is a fast-growing area of dentistry. Of the approximately 40 million people in the U.S. with obstructive sleep apnea (OSA), 90% are undiagnosed. Simply put, obstructive sleep apnea is a medical condition whereby a physical obstruction (for example, tongue or pharyngeal muscles) blocks the airway, which stops the patient from breathing while he or she sleeps. Patients with OSA will have multiple apneas/hypopneas every night while they sleep, which can severely impact their health. OSA is comorbid with and dramatically increases the incidence and severity of diabetes, hypertension, stroke, and heart attacks in patients (and let's not forget that dentists are patients too).
Bruxism, TMJ, and orofacial pain are also very commonly comorbid with OSA. As a matter of evidence-based fact, sleep-disordered breathing causes bruxism. The connection is this: What is the brain's mechanism to get patients to breathe when they have a blocked airway causing an apnea? The brain needs to open the airway and get the muscles of mastication to start working hard and fast, a process we know as bruxism. The masticatory muscles move the jaw forward, the airway opens, and the patient takes in a deep rescue breath. The patient falls back asleep, the airway gets blocked, and the process repeats many times during the night. This is known in evidence-based studies assleep bruxism.
This same patient wakes up in the morning with a headache and jaws and facial muscles that hurt. The patient comes to your office with TMJ. It is clear that he or she is bruxing. If you don't have any knowledge about OSA or whether or not the pain is being caused by the patient's TMJ or head and neck muscles, how would you know what kind of appliance to make? Let's say your patient has OSA and you choose your favorite bruxism appliance, which may position the mandible backwards. I hope by now you realize that this "bruxism" appliance will now close the patient's airway at night, which makes the OSA worse and results in more bruxism - not less. Additionally, if the orofacial pain is coming from either the TM joint and/or muscle trigger points and you make the wrong kind of appliance, the pain gets worse-not better.
Don't waste your money
In the past, many dentists have invested in a home sleep monitor or other expensive equipment that only measures for OSA. In my opinion, that is a waste of resources. Why would a dentist invest in a piece of equipment for a medical condition you can't even legally diagnose? You have to refer the patient to a physician with the sleep results, and the physician has no reason to send the patient back to you but instead refers to a sleep lab. The dentist cannot demonstrate any dental condition that would justify the physician sending the patient back to the dentist. An investment like this would only make sense if the home testing unit would also give the dentist objective measurements concerning bruxism and OSA together.
There has been an exciting advancement in the areas of bruxism and dental sleep medicine that will now allow a dental clinician to objectively collect data to measure bruxism and OSA in patients. Figure 1 shows the STATDDS Bruxism and Sleep Monitor (STATDDS.com), a very cost-effective home test that the patient wears at night while sleeping. The AAFE dental sleep medicine training course exclusively uses this home monitor because of its ability to test for bruxism.
The exclusive software that comes with this monitor is made specifically for dentistry to analyze the testing data and give the dentist a simple-to-understand report with the patient's bruxism episodes index (BEI) and the apnea/hypopnea index (AHI). The BEI measures the number of bruxism episodes per sleep hour and the AHI measures how many apnea/hypopneas per sleep hour. The monitor can be purchased or rented by the dental practice. Each home test costs less than $20 to administer. Currently, this is the only monitor of its kind with specialized software that has been specifically configured to analyze both the BEI and AHI and produce patient-specific reports for dental offices.
Using objective evidence
Here are two cases showing how to use objective bruxism measurements for treatment planning and best therapeutic outcomes.
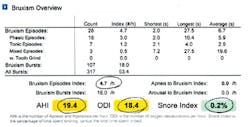
Figure 2- Objective test results show bruxism and very significant OSA caused by wearing appliance.
Case 1 - A patient was wearing a bruxism appliance and his orofacial pain wasn't getting better. Take a look at Figure 2 where you can see the initial STATDDS home bruxism and sleep test report. You can see that the patient has a BEI of 4.7, which means the patient has significant bruxism activity in his muscles even while wearing the appliance. From a bruxism standpoint, the appliance may be somewhat effective; we don't know until there is a baseline report without the appliance. Now, let's look at the AHI number, which tells us about the patient's airway and obstructive sleep apnea: It is a very worrisome 19.4.
Let's analyze this data objectively. The appliance may or may not be working for bruxism, and is causing or exacerbating the patient's obstructive sleep apnea. Now I can personally tell you that in more than 35 years of dental practice, I have never seen a patient die of bruxism, but they do die of complications related to obstructive sleep apnea. This report clearly indicates that this particular appliance is not only inappropriate for this patient, but it can be potentially dangerous as well.
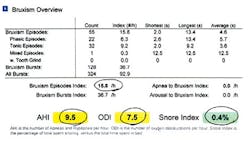
The treating dentist decided to use the STATDDS monitor to test this patient again, and this time the patient did not wear the appliance overnight. Figure 3 shows the test results. The BEI number is now 15.8, and the AHI is 9.5. There is no question that this patient is a very destructive bruxer, so this needs to be addressed. We now see the oral appliance was helping the bruxism, but at the great expense of exacerbating a dangerous medical problem. It is also clear that the patient does have obstructive sleep apnea, which needs to be officially diagnosed by the patient's physician.
Based on this patient's data, the treatment choice is now clear and data-driven. The dentist calls the patient's physician, sends a copy of the report, and has a discussion. The patient has very serious bruxism, TMD, and orofacial pain. The physician is shown the OSA numbers. The dentist and physician are coproviders on this patient who has crossover treatment needs. The dentist informs the physician that they can make an oral appliance that can address both conditions successfully and will do follow-up testing. The physician will gladly give the dentist an Rx for an oral appliance that can be billed to medical insurance/Medicare by the dentist. A mandibular advancement device, which also will double as a bruxism appliance, is the device of choice for this patient. It is important to note that not all oral appliances for dental sleep medicine are appropriate for bruxers; training is needed to understand which appliances best fit each clinical situation based on the obtained data.
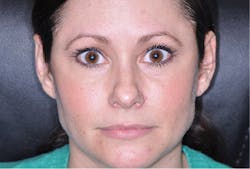
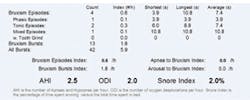
Case 2 - This patient is a good example of the demonstrable success that we can now measure with objective evidence. Thousands of dental professionals are now using botulinum toxin (Botox/Xeomin) for relief of bruxism and orofacial pain. With the STATDDS monitor, we can now quantify the successful results as well as manage the dosage needed depending on the test results. Figure 4 shows the preop photo of a patient who has a 10-year history of orofacial pain. Her test results show a BEI of 5.2 and an AHI of 4.8 shown in Figure 5. After trigger point injections with approximately 60 units of botulinum toxin, Figure 6 shows her postoperative test and the results are impressive - the patient's BEI falls to 0.6. Interestingly, the patient's AHI also falls significantly. Both the BEI and AHI results in patients are a development currently being studied by the AAFE in a multilocation study. Figure 7 shows the patient's esthetic result as a result of the therapeutic injections that are associated with botulinum toxin as well as the elimination of the patient's orofacial pain for the first time in 10 years. Cases like this clearly show both the patient and the clinician how successful botulinum toxin therapy can be in the treatment of bruxism and orofacial pain. I use botulinum toxin routinely in most of my restorative cases to control the masticatory muscles to achieve long-term success for the dentistry I place in patients' mouths. With the ability to now obtain objective and reliable data, I can now quantify and titrate my botulinum toxin dosing for maximum effectiveness.
Training is essential in the areas of orofacial pain, dental and facial esthetics, dental sleep medicine, and oral appliances for bruxism therapy before a dentist ever makes another "bruxism" appliance. Many "bruxism" appliances that are currently being made negatively impact a patient's health if you do not understand the impact these appliances have on the TMJ, orofacial pain, and OSA. Successful restorative, bruxism, and orofacial pain treatment have now entered a new era with the use of cost-effective qualitative testing, botulinum toxin, and the relationship of oral appliances to OSA. Many of these treatments are also reimbursable by the patients' insurance companies. It is time for dentistry to catch up with medicine in its ability to objectively measure and use data to help diagnose and more effectively treatment plan for the best therapeutic pain and restorative outcomes for our patients.
Louis Malcmacher, DDS, MAGD, is a practicing general dentist and an internationally known lecturer and author. He is president of the American Academy of Facial Esthetics (AAFE). Contact him at (800) 952-0521 or email drlouis@facialesthetics.org. Go to www.FacialEsthetics.org for information about live patient Frontline TMJ/Orofacial Pain training, Frontline Dental Sleep Medicine, Bruxism Therapy and Medical Insurance, Botox and dermal fillers training, download his resource list, and sign up for a free monthly e-newsletter.