Implant complications: multiple treatment modalities; few financial options
By Scott Froum, DDS, and Kyle L. Summerford
Although the high predictability and long-term success rate of dental implants is well documented in the literature, complications and failures do occur. Success and predictability of dental implants have been well documented throughout the years with purported success rates of more than 90%. (1)1 These success rates, however, have been established according to an older criteria. An implant without pain, mobility, radiolucency, or 1 mm of bone loss during the first year and .2 mm thereafter was considered a success.(2) A recent review that considered excessive bone loss as an additional criteria of implant failure suggested that "implant survival and success rates in general dental practices may be lower than those reported in studies conducted in academic or specialty settings" and quoted an 80% success rate.(3) In addition, proportional with the increase in the volume of dental implants being placed is the amount of adverse events that will occur. Two recent systematic reviews and meta-analyses reported that the prevalence of peri-implantitis was present in approximately 10% of implants and 20% of patients eight to 10 years after implant placement.(4) Considering the number of implants placed or projected to be placed from 2013 to 2017 in the United States alone, this number would mean more than 1.2 million implants will require therapy for this disease.(5)
Some complications may be relatively minor and easy to correct, while others will be major and result in the loss of the implant or prosthesis. Implant complications can typically be categorized by temporal sequence and defined as either an early or late complication. An early complication can be defined as a problem that arises prior to osseointegration of the dental implant, whereas a late complication occurs after the implant osseointegrates and the final prosthesis is placed. In addition, implant problems can further be subcategorized into biologic or mechanical complications. Biologic complications involve pathosis of the peri-implant hard and soft tissue. Mechanical complications occur when the fatigue strengths of the dental implant or restorative components are reached and breakdown occurs resulting in material failure.
Early implant complications arise prior to dental implant integration and often are the result of intraoperative or short-term postoperative problems. Typical early complications include intrasurgical problems such as hemorrhage, damage to adjacent teeth, neurosensory disturbances, jaw fracture, and maxillary sinus violations. Other early complications during implant placement include overpreparation of the implant osteotomy or underpreparation of the implant osteotomy. Underpreparing an implant site can result in surgically overheating the bone and bone necrosis if the critical threshold of greater than 47°C is reached by the surgical drills or dental implant.(6) Contamination of the surgical site and/or the dental implant surface from bacteria is also possible during fixture placement, which can result in the failure of the implant to integrate. Lack of primary stability, stability of the implant when it is first placed into the alveolus, can result in implant micro-motion above 100 microns and loss of the implant due to fibrous tissue bonding to the implant surface instead of bone.(7)
Late implant complications occur after the implant has integrated and the final prosthesis has been placed. Recognition of these complications via radiographic and clinical analysis is extremely important since many of these problems can be corrected if detected early. On the other hand, if allowed to progress, a minor complication can often result in loss of the implant and/or prosthesis. Late complications of the dental implant fall into the category of biologic or mechanical complications. Late biologic complications are those in which the peri-implant soft and hard tissues are affected. Peri-implant mucositis describes a reversible inflammatory reaction in the mucosa adjacent to an implant,(8) a term that has become known as implant gingivitis. Studies show that the prevalence of peri-implant mucositis can be as high as 50% to 80% of implants in function(9) with the etiology of peri-implant mucositis being bacterial plaque. Typical clinical presentation includes erythema, edema, swelling, and redness (Figs. 1 and 1a). Although bleeding upon probing and increased probing depths are not always indicative of peri-implant mucositis,(10) the absence of these two factors usually means implant health.(11)
Treatment of peri-implant mucositis can often be accomplished via nonsurgical mechanical therapy. Although systemic antibiotics have been shown to reduce inflammation associated with peri-implant gingival tissue, as a monotherapy, they have been shown to be ineffective due to the bacterial recolonization of the implant surface without mechanical debridement.(12) Studies show that proper scaling and root planing with attention to bacterial plaque removal can be effective in reducing peri-implant mucositis lesions.(13) Localized drug delivery has also shown to have a positive effect in reducing mucositis lesions in conjunction with mechanical debridement (Fig. 2), especially in the areas of the mouth that are hard to reach.(14) After nonsurgical intervention, the patient should be recalled within three weeks. If no resolution of the inflammation has occurred, surgical intervention should occur.(15)
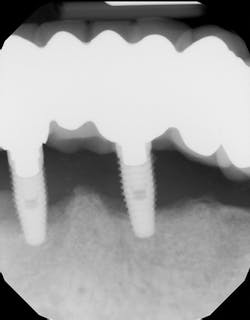
Peri-implantitis has been defined as an inflammatory process that affects the tissues around an osseointegrated implant in function and, like periodontitis, results in loss of supporting bone6 (Figs. 3 and 3a). The prevalence of peri-implantitis has been shown in some studies to range from 11% to as high as 47% of implant sites analyzed.(16) Most literature reviews agree that once bone loss has occurred around an implant, nonsurgical therapy is not as effective as surgical treatment.(17) Surgical intervention by the dentist or specialist includes raising a full thickness flap around the affected dental implant in order to completely expose the dental implant surface (Fig. 4). Mechanical debridement with hand and high-speed instrumentation as well as irrigation with various medicaments is advocated in order to detoxify the implant surface and alleviate bacterial contamination. After decontamination, the flap can be apically or coronally positioned. In addition, various regenerative technologies, including bone and soft-tissue grafts, growth factors, and barrier membranes have been used to rebuild lost tissue support around the dental implant (Figs. 5 and 5a). Different methods of guided bone regeneration around implants affected with peri-implantitis were demonstrated, and the results have been shown to be stable for a follow-up period of up to seven years.(18) That being said, no gold standard of peri-implant disease has been documented and "available evidence does not allow specific recommendations for the therapy of peri-implantitis."(19)
With a better understanding of the many treatment modalities available to treat peri-implant disease, we now have to consider the limited financial options a patient has when paying for this treatment. Of course, fee-for-service with no insurance involvement is the preferable method of payment. This, however, may be cost prohibitive when the surgical methods of treatment often accompany bone grafts and/or membranes, biologics, soft-tissue grafts, and other augmentation materials. Insurance reimbursements and involvement are often solutions to help patients have access to peri-implant disease treatment. Insurance submissions and obtaining approvals are often confusing when it comes to peri-implant treatment. The first step in understanding the tangled web of insurance is to understand that insurance companies have created their own definition and standard of treatment for peri-implant disease. Insurance companies do not recognize peri-implant mucositis, only peri-implantitis. In addition, most insurance companies will only accept treatment in the form of surgical access, debridement, and flap replacement without the use of regenerative treatment. For example, this was taken directly off of Aetna Dental's website: "Despite large numbers of publications available regarding peri-implantitis treatments, there are no long-term studies which indicate that the uses of osseous contouring, placement of barriers or bone grafts are superior to flap reflection with debridement. Therefore, Aetna considers flap reflection with debridement as the accepted clinical protocol for peri-implantitis treatment."
The key to having treatment covered by insurance companies and giving the patient a chance at reimbursement is to use the correct ADA 2013 and 2014 CDT codes, which have been updated and include quite a few dental codes billed directly to insurance companies for the treatment of peri-implant disease. The following codes are the correct codes used for implant services:
• D6100 - implant removal, by report (include supporting narrative)
• D6101 - debridement of a peri-implant defect and surface cleaning of exposed implant surfaces, including flap entry and closure
• D6102 - debridement and osseous contouring of a peri-implant defect; includes surface cleaning of exposed implant surfaces and flap entry and closure
• D6103 - bone graft for repair of peri-implant defect - not including flap entry and closure or, when indicated, placement of a barrier membrane or biologic material to aid in osseous regeneration
• D6080 - implant maintenance procedures when prostheses are removed and reinserted, including cleansing of prostheses and abutments
Despite many of the dental insurance companies' exclusions and limitations on covering the costs associated with treatment of peri-implantitis, if the correct codes are used, payment may be rendered. Of course, the terms of carriers and groups of different contracts vary. Unless the patient's insurance group contract specifies implants are an actual covered benefit, the fees for implant services will be denied entirely. It becomes imperative that staff members check the insurance plan of the patient prior to any treatment recommendation or case presentation to determine whether implant services are a covered or noncovered benefit.
Below are examples of two recent patients who were diagnosed with peri-implantitis in which preauthorizations were filed with three major dental insurance carriers. Each patient's dental plan indicated that each group policy contained implants and related services as an actual covered benefit.
Example No. 1. Patient A: |
Treatment approved by primary insurance (Delta Dental): D6101 - debridement of peri-implant defect and surface cleaning of exposed implant surfaces, including flap entry and closure |
Treatment denied by primary insurance (Delta Dental): D6103 - bone graft for repair of peri-implant defect - not including flap entry and closure or, when indicated, placement of a barrier membrane or biological material to aid in osseous regeneration |
Treament approved by secondary insurance (Aetna Dental): D6080 - implant-maintenance procedures, including removal of prosthesis, cleansing of prosthesis, and abutments and reinsertion of prosthesis |
Treatment denied by secondary insurance (Aetna Dental): D6101 - debridement of a peri-implant defect and surface cleaning of exposed implant surfaces, including flap entry and closure D6103 - bone graft for repairof peri-implant defect - not including flap entry closure or, when indicated, placement of a barrier membrane or biological material to aid in osseous regeneration |
Example No. 2: Patient B: |
Treatment denied by sole insurance company (MetLife Dental): D6103 - bone graft for repair of peri-implant defect - not including flap entry and closure or, when indicated, placement of a barrier membrane or biologic material to aid in osseous regeneration D6101 - debridement of a peri-implant defect and surface cleaning of exposed implant surfaces, including flap entry and closure |
Treatment approved by sole insurance company (MetLife Dental): D6080 - implant-maintenance procedures, including removal of prosthesis, cleansing of prosthesis, and abutments and reinsertion of prosthesis |
As we see, there seems to be a misunderstanding in the gold standard approach when it comes to a uniformed policy for dental insurance coverage in relation to the treatment of peri-implantitis.
The presented ADA codes are still very new, and the following table is an average of multiple well-known insurance companies' usual customary rate (UCR) for different implant disease services based on zip codes for the following major cities located throughout the United States.
New York City: 10022
Los Angeles: 90067
Chicago: 60604
It should be emphasized that regardless of the treatment modality, a prerequisite for successful therapy is the establishment and maintenance of proper home-care practices and supportive care at regular intervals. This has been documented in the literature with respect to both periodontal and peri-implant maintenance and treatment outcomes. Many studies suggest that patients who are placed on three-month recare schedules typically perform better than those seen on longer intervals and tend to keep their teeth for longer periods of time.20 Optimal home care, short maintenance intervals, and proper treatment are keys to success when dealing with peri-implant disease. In addition, treatment, whether nonsurgical or surgical intervention, must be performed in a timely manner. Sacrifices in treatment or delay of services should not occur, because the progression of this disease can be quick in nature. Accurate peri-implant coding and submissions when dealing with insurance companies are a must to facilitate services and expedite reimbursements.
TABLE 1:
| Peri-Implantitis Procedure | New York City | Los Angeles | Chicago |
| Implant removal (by report) | $500 | $475 | $500 |
| Debridement peri-implant defect | $350 | $200 | $350 |
| Debridement/osseous peri-implant defect | $475 | $375 | $450 |
| Bone graft repair/ peri-implant defect | $675 | $550 | $675 |
| Implant maintenance procedures | $300 | $150 | $275 |
Kyle L. Summerford is an independent dental consultant. His professional career of 13 years in dentistry has given him expert knowledge in various areas of practice management. He is a professional speaker focusing on various topics such as increasing profits, staff etiquette training, and maximizing dental insurance benefits. He has authored many articles that have been featured in Dental Economics, DentistryIQ.com, and Perio-Implant Advisory. Visit his websites at www.ddsguru.com and www.rescuemydentalpractice.com, available to dentists and team members for educational purposes. You may contact Mr. Summerford by email at [email protected] with any inquiries regarding his practice management consulting services.
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of the American Board of Periodontology, is a clinical associate professor at SUNY Stony Brook School of Dental Medicine in the Department of Periodontology. He serves on the board of editorial consultants for the Academy of Osseointegration's Academy News. Contact him through his website at drscottfroum.comor (212) 751-8530.
References
1. Adell R, Lekhom U, Rockler B. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981;10:387.
2. Albrektsson T, Zarb G, Worthington P. The long-term efficacy of currently used dental implants. A review and prognosis criteria for success. Int J Oral Maxillofac Implants 1986;1:11.
3. Da Silva JD et al. Outcomes of implants and restorations placed in general dental practices: A retrospective study by the Practitioners Engaged in Applied Research and Learning (PEARL) Network. JADA. July 1, 2014;145:704-713.
4. Mombelli A, et al. The epidemiology of peri-implantitis. Clin Oral Implants Res. 2012;23(Suppl. 6):67-76.
5. 2013-2017 US Dental Implant Market iData Research Inc. 2013.
6. Esposito M, Hirsch J, Lekholm U, et al. Biological factors contributing to failures of osseointegrated oral implants. I. Success criteria and epidemiology. Eur J Oral Sci 1998;106:527.
7. Brunski JB. Biomechanical factors affecting the bone-dental implant interface. Clin. Materials 1992;10:153-201.
8. Albrektsson T, Isidor F. Consensus report of session IV. In: Lang NP, Karring T, ed. Proceedings of the First European Workshop on Periodontology. London: Quintessence, 1994:365-369.
9. Lindhe J, Myle J. Peri-implant diseases: Consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontology 2008;35(suppl 8): 282-285.
10. Ericsson I, Lindhe J. Probing at implants and teeth: An experimental study in the dog. J Clin Periodontol 1993;20:623-627.
11. Salvi G, Lang N. Diagnostic parameters for monitoring peri-implant conditions IJOMI 2004;19(SUPPL):116-127.
12. Mombelli A, van Oosten MA, Schurch E, Lang NP. The microbiota associated with successful or failing osseointegration titanium implants. Oral Microbiology and Immunology. 1987;2:145-151.
13. Roos-Jansaker AM, Renvert S, Egelberg J. Treatment of peri-implant infections: a literature review. J Clin Periodontol 2003;30:467-485.
14. Renvert S. Nonsurgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Perio Sept. 2008;35(8 Suppl):305-315.
15. Heitz-Mayfield LJA et al. The therapy of peri-implantitis: A systematic review. Int J Oral Maxillifac Implants 2014;29(suppl):325-345.
16. Koldsland O et al. Prevalence of peri-implantitis related to severity of the disease with different degrees of bone loss. J Perio Feb. 2010; 81(2)231-238.
17. Kotsovilis S, Karoussis IK, Triant M, Fourmoseuses I. Therapy of peri-implantitis: A systemic review. J Clin Periodontology 2008;35:621-629.
18. Froum SJ, Froum SH, Rosen P. Successful management of peri-implantitis with a regenerative approach: A consecutive series of 51 treated implants with 3- to 7.5-year follow-up. IJPRD Feb. 2012; 32(1).
19. Chan H et al. Surgical treatment of peri-implantitis: A systematic review and meta-analysis. Accepted for publication J. Perio 2015.
20. Wilson TG Jr. Maintaining periodontal treatment. J Am Dent Assoc. 1990;121(4):491-494.