When to do heroic repairs of fixed prostheses
by Gordon J. Christensen, DDS, MSD, PhD
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics® readers. If you would like to submit a question to Dr. Christensen, please send an email to [email protected].
Q One of the most frustrating clinical situations I encounter is deciding what to do when a fixed prosthesis fails and the patient does not have the financial resources to place a new one. Repair of the previously placed prosthesis is possible, but the outcome is questionable and the procedure is difficult. How do you handle these situations?
A We often face this clinical challenge. One of the unavoidable weaknesses of dental education is that dental students usually do not see typical clinical failures while in school. Almost every treatment they provide in school is observed for only one or two years. As a result, most graduates don't have the experience to learn when and how to repair or redo restorations.
I will use a recently treated patient to assist in providing my thoughts and opinions with regard to your question, because the patient I show in this article appears to have the challenges you expressed.
A few years before the failure of the patient's fixed prosthesis, I placed a cantilever fixed prosthesis (FPD) from the maxillary left canine to an abutment on the first premolar and extending to a cantilever replacing the second premolar. Why did I not place implants in this case? There was not adequate bone present without significant grafting, and the patient had limited financial resources.
Several years later, the patient suffered a serious car accident in which the fixed prosthesis received a significant blow, and coronal portions of the abutment teeth were broken from the roots. Fig. 1 shows the inadequacy of bone present in the areas for potential implant placement.
Figs. 2 and 3 show the cantilever fixed prosthesis after the accident. It appears to be intact and without ceramic fracture from the metal substructure.
I did not see the patient for several weeks after the accident, as she was recovering and did not have discomfort from the broken-off teeth.
During that time, the gingiva had partially grown over the broken-off roots (Fig. 4). Placement of the original FPD was difficult, as the patient did not want a removable prosthesis, thus requiring the use of the cantilever instead. After the accident, the clinical situation was even more difficult, and the patient's financial situation was worse than before. The alternatives were not good. They included:
- Extract or restore the broken teeth and place a maxillary removable partial denture. She vehemently did not want a removable prosthesis.
- Accomplish difficult, expensive, and relatively unpredictable sinus grafting and hope it works. Then place implants and a fixed prosthesis. Financial limitations precluded this treatment.
- Attempt to salvage the fixed prosthesis. The patient wanted to attempt salvaging the fixed prosthesis. What limitations and precautions should we tell patients when accomplishing a difficult and relatively unpredictable salvage? They should be assured that we will do our best to make the procedure successful.
Make the patient aware of the following:
- Caution patients that events may occur during the salvage that show it is impossible or impractical to continue with the procedure.
- Warn patients that the salvage may not be as strong as the original restoration.
- Explain that other treatments may be better and stronger, but will cost more.
Place this information in the patient's file for future verification, and make sure you obtain written informed consent for the repair.
The following clinical procedure was accomplished for the example patient:
- Gingival tissue that had grown over the broken-off teeth was removed using electrosurgery.
- The teeth were cleaned well with flour of pumice on a rotary rubber cup.
- Endodontic treatment was accomplished on the canine, which was nonvital (Fig. 5).
- The first premolar was vital, and it was decided not to accomplish endodontic treatment on it. The patient was advised of this decision and warned of potential future endodontic need.
- A fiber-reinforced, resin-based composite post (Pentron FibreKleer) was placed into the canine tooth, and the FPD was tried onto the tooth preparation to ensure that the post was not too long coronally.
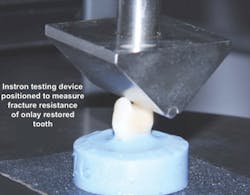
- Pure titanium pins, 0.025 inch in diameter (Filhol Filpins), were placed one at a time circumferentially around the canine and the first premolar. Pins should not be parallel with one another when placed into the dentin since dentin relaxes during service and parallel pins have been shown to pull out of the dentin. They should be at least 15 degrees nonparallel with one another. After each pin was placed and bent into the center of the tooth, the FPD was again tried in to check that it seated adequately (Fig. 6).
- The remaining debris on the inside of the abutment crowns was removed, and the internal of the FPD was roughened and sandblasted to provide mechanical retention (Fig. 7).
- Before cementation, the tooth preparations received an application of a glutaraldehyde/HEMA solution (Danville Materials MicroPrime) for disinfection and desensitization. Two one-minute applications disinfect the tooth preparations thoroughly.
- Before cementation, the FPD was placed onto the tooth preparations. The occlusion and margins were checked to ensure that the FPD was seating all the way onto the preparations.
- Any moderate viscosity resin buildup material could have been used to attach the FPD to the retentive features provided on the tooth preparations. In this case, I used Ivoclar MultiCore Flow. It is a self-cure and/or light-cure material. The FPD was seated, followed by a careful evaluation of the margins and occlusion before the material set (Figs. 8 and 9).
- The patient was advised of the service expectations and the need to be cautious when eating tough or hard foods.
This grateful patient was very satisfied not to have to undergo the other alternative treatments. To date, the salvaged FPD is serving well.
Fees for repair of restorations
What should repair of a fixed prosthesis cost the patient? Every repair is different! For the example patient, several normal fee categories were present, including exam, radiographs, endodontic treatment, pin placement, post and core, and recementation of the FPD. If you add up typical fees for those procedures, it becomes clear that the total amount is adequate for the 30 or 40 minutes required to accomplish the repair.
Longevity of repairs
As stated above regarding fees, every repair has a different longevity expectation. The longevity is related to many factors, including patient oral hygiene, occlusion, the severity of the original failure, the patient's care in chewing after the repair, and your own expertise in accomplishing the repair. Patients should be advised of the relative uncertainty of any repair. Most patients have chosen and accepted the repair instead of other alternatives because they have financial limitations and/or they do not want more extensive treatment. In cases where the repair also fails, I have found that patients come back because they respect you for giving them some years of service that they otherwise would not have had.
Summary
When failure of a fixed prosthesis occurs, patients should be offered all of the alternatives. Often, because of many factors, mainly financial limitations, they elect to repair the restoration. The patient should be provided with realistic expected outcomes for any repair and knowledge that a repair is somewhat unpredictable. Most patients are pleased and grateful when you repair a fixed prosthesis and they will continue to remain in your practice.
Gordon Christensen, DDS, MSD, PhD, is a practicing prosthodontist in Provo, Utah. He is the founder and director of Practical Clinical Courses, an international continuing-education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Dr. Rella Christensen) and CEO of CLINICIANS REPORT (formerly Clinical Research Associates).
Additional education on repairing restorations
Recently we made a detailed video presentation on many different types of repairs for fixed restorations. Our one-hour DVD,
How to Repair and Maintain Fixed Restorations (Item #V1961),
is the second edition we have produced because very little information is available on this topic and repairs are often needed.
Contact Practical Clinical Courses at 800-223-6569, or visit our website www.pccdental.com for further information.
Past DE Issues